Highlights
- Intramuscular administration of AMG0001 significantly reduced the median time to complete ulcer healing from 280 days in the placebo group to 84 days in the treatment group (P=0.007).
- Long-term efficacy was robust, with 77.6% of AMG0001-treated participants achieving complete healing by 12 months, compared to only 46.2% in the placebo arm.
- The study highlights the potential of ‘anatomically directed’ delivery, using angiography to guide plasmid injections along specific arterial pathways to optimize therapeutic angiogenesis.
- AMG0001 demonstrated a favorable safety profile, with adverse event rates comparable to placebo, supporting its development as a nonsurgical option for moderate CLTI.
The Burden of Chronic Limb-Threatening Ischemia
Chronic limb-threatening ischemia (CLTI) represents the end-stage of peripheral artery disease (PAD), characterized by rest pain, non-healing ulcers, or gangrene. For patients with CLTI, the risk of major amputation and cardiovascular mortality is exceptionally high. Despite advances in endovascular and surgical revascularization, a significant proportion of patients—often termed ‘no-option’ patients—are poor candidates for traditional procedures due to lack of suitable conduit vessels, diffuse infrapopliteal disease, or prohibitive surgical risk.
The clinical challenge is particularly acute in patients with neuroischemic ulcers, where both impaired perfusion and peripheral neuropathy contribute to a hostile wound-healing environment. Currently, there are no FDA-approved pharmacologic or biologic therapies specifically indicated to promote wound healing in this population. Previous attempts at therapeutic angiogenesis using protein or gene-based growth factors have yielded inconsistent results, often failing to meet primary endpoints in late-phase trials. The LEGenD-1 trial sought to address these past failures by utilizing a more precise, anatomically directed delivery method and focusing on a specific subset of patients with moderate ischemia.
LEGenD-1: Study Design and Methodology
Patient Selection and Randomization
LEGenD-1 was a phase II, double-blind, randomized, placebo-controlled trial conducted across 22 sites in the United States. The study enrolled 75 participants with CLTI and neuroischemic ulcers. Inclusion criteria were stringent, focusing on ‘moderate’ ischemia defined by a toe pressure or transcutaneous oxygen pressure (TcPO2) between 30 and 59 mm Hg. This range represents a population that, while ischemic, may still possess sufficient microvascular reserve to respond to regenerative signals.
Participants were randomized in a 1:1:1 ratio to receive either a low-dose (4 mg) of AMG0001, a high-dose (8 mg) of AMG0001, or a placebo. AMG0001 is a plasmid DNA encoding the human hepatocyte growth factor (HGF) gene. HGF is a potent angiogenic and lymphangiogenic factor that promotes endothelial cell proliferation and migration while also exerting anti-apoptotic and anti-inflammatory effects.
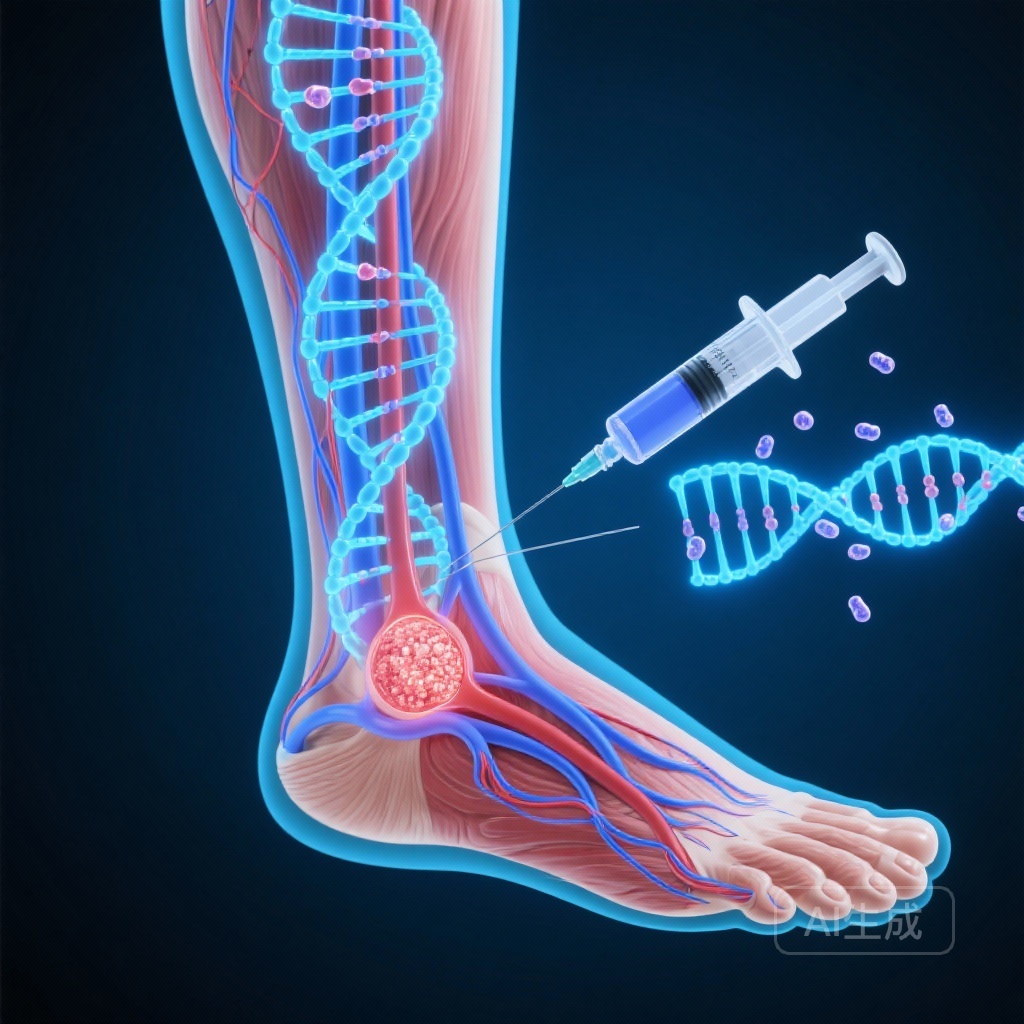
The Intervention: Anatomically Directed Delivery
A distinguishing feature of the LEGenD-1 trial was its delivery strategy. Unlike prior studies that used standardized grid-like injection patterns, LEGenD-1 utilized anatomically directed intramuscular injections. Clinicians used baseline angiography to identify the target artery providing primary flow to the ulcerated area. The AMG0001 or placebo was then injected along the path of this specific artery on days 0, 28, 56, and 84. This approach aimed to concentrate the therapeutic agent where it was most likely to enhance the regional collateral network.
Study Endpoints
The trial employed two coprimary endpoints: the time to complete healing of the target ulcer and the proportion of subjects with completely healed ulcers at 6 months (pooled AMG0001 analysis). Secondary endpoints included healing rates at 12 months, ulcer recurrence, and changes in hemodynamic parameters such as toe pressure and TcPO2.
Key Findings: Accelerating the Path to Healing
Primary Outcomes and Accelerated Healing
The results of the LEGenD-1 trial demonstrated a clear and statistically significant benefit for patients receiving AMG0001. The median time to complete ulcer healing was substantially shorter in the pooled AMG0001 group (84 days) compared to the placebo group (280 days; P=0.007). When broken down by dose, both the 4 mg group (98 days; P=0.017) and the 8 mg group (84 days; P=0.022) outperformed placebo, suggesting a robust therapeutic effect across the tested dosage range.
At the 6-month mark, 63.3% of the AMG0001-treated participants had achieved complete healing, compared to 38.5% in the placebo group. While this narrowly missed the traditional threshold for statistical significance for the 6-month proportion (P=0.053), the clinical trend was strongly in favor of the gene therapy.
Long-term Efficacy and Durability
The secondary endpoint of healing at 12 months provided even more compelling evidence of durability. By one year, 77.6% of the AMG0001 group had healed, versus only 46.2% of the placebo group (P=0.010). This widening gap suggests that the biological changes induced by HGF gene therapy may have lasting effects on the local microenvironment, facilitating complete tissue restoration in patients who otherwise struggle with chronic, recalcitrant wounds.
Safety and Tolerability
Safety is a paramount concern in gene therapy trials. In LEGenD-1, AMG0001 was well-tolerated. The incidence of treatment-emergent adverse events (TEAEs) was similar across the three groups. Most adverse events were related to the underlying disease process or the injection procedure itself, rather than the plasmid DNA. Importantly, there were no signals of increased oncologic risk or pathological angiogenesis (such as proliferative retinopathy), which are theoretical concerns with growth factor therapies.
Expert Commentary: Mechanistic Insights and Clinical Implications
The Role of Hepatocyte Growth Factor (HGF)
The success of LEGenD-1, where others have failed, may be attributed to the specific biological properties of HGF. Unlike vascular endothelial growth factor (VEGF), which can sometimes produce ‘leaky’ or immature vessels, HGF promotes the formation of more stable, mature vasculature by acting on both endothelial cells and pericytes. Furthermore, HGF’s role in reducing fibrosis and promoting tissue regeneration makes it particularly suited for the complex pathology of neuroischemic ulcers.
The Precision Medicine Approach in CLTI
The ‘anatomically directed’ injection technique represents a shift toward precision medicine in vascular surgery. By tailoring the delivery to the patient’s specific anatomy, clinicians can maximize the ‘area under the curve’ for growth factor expression in the tissues that need it most. This methodological refinement likely contributed to the significant reduction in healing time observed in this study.
Study Limitations
While the results are promising, the trial’s small sample size (n=75) is a limitation. As a Phase II study, it was designed to identify signals of efficacy and safety rather than provide definitive evidence for regulatory approval. Additionally, the study focused on moderate ischemia (TcPO2 30-59 mmHg); whether these results can be extrapolated to ‘no-option’ patients with more severe ischemia (TcPO2 < 20 mmHg) remains to be determined.
Summary and Clinical Takeaways
The LEGenD-1 trial marks a significant milestone in the development of biologics for chronic limb-threatening ischemia. By demonstrating that AMG0001 can reduce the median time to ulcer healing by nearly 200 days, the study offers hope for a potent, nonsurgical intervention to prevent the devastating progression of CLTI. For clinicians, these findings suggest that gene therapy, when combined with precise anatomical targeting, may soon become a vital component of the limb salvage toolkit.
The next steps will involve larger Phase III trials to confirm these findings and further define the patient populations most likely to benefit. If these results hold, AMG0001 could redefine the standard of care for neuroischemic ulcers, shifting the focus from wound management to active biological healing.
Funding and Registration
The LEGenD-1 trial (NCT04267640) was sponsored by AnGes, Inc. The researchers and sites involved were supported by grants and institutional funding dedicated to vascular regenerative medicine.
References
Armstrong DG, Conte MS, Mills JL, Menard MT, Orgill DP, Galiano RD, Kirsner RS, Farber A, Lantis JC, Zelen CM, Carter MJ, Hicks CW, Powell RJ. Anatomically Directed Lower Extremity Gene Therapy for Ulcer Healing: A Double-Blind, Randomized, Placebo-Controlled Study (LEGenD-1). Circ Cardiovasc Interv. 2026 Jan;19(1):e015648. doi: 10.1161/CIRCINTERVENTIONS.125.015648. Epub 2025 Nov 4. PMID: 41186002.