Highlights
- Metopimazine mesylate (NG101), a peripherally restricted dopamine D2 receptor antagonist, demonstrated a favorable safety profile over 12 weeks of treatment.
- The primary endpoint of reducing mean nausea severity on the DIGS-DD scale was not met with statistical significance compared to placebo.
- Significant improvements were observed in the Patient Global Impression of Change (PGIC) for nausea across all dose groups (5, 10, and 20 mg).
- Subgroup analysis suggests that patients with idiopathic gastroparesis may derive greater benefit from NG101 than those with diabetic gastroparesis.
Introduction: The Unmet Need in Gastroparesis Management
Gastroparesis is a chronic, debilitating neuromuscular disorder of the upper gastrointestinal tract characterized by delayed gastric emptying in the absence of mechanical obstruction. Clinically, it manifests as a constellation of symptoms including nausea, vomiting, postprandial fullness, early satiety, and abdominal pain. The impact on quality of life is profound, often leading to nutritional deficiencies, frequent hospitalizations, and significant psychological distress.Despite the high disease burden, therapeutic options remain severely limited. Metoclopramide, the only FDA-approved medication for gastroparesis, is fraught with concerns regarding its central nervous system (CNS) effects, specifically the risk of tardive dyskinesia, which has led to a black box warning. Domperidone, while effective, is not FDA-approved and requires an Investigational New Drug (IND) application for use in the United States due to concerns over QT interval prolongation. Consequently, there is an urgent clinical need for a prokinetic and antiemetic agent that provides efficacy without the neurological or cardiac risks associated with existing D2 antagonists.
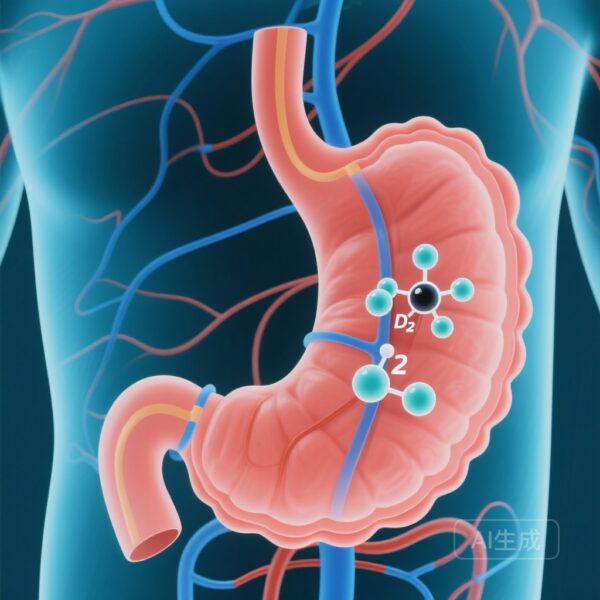
Metopimazine Mesylate: A Peripherally Restricted Strategy
Metopimazine is a selective dopamine D2 receptor antagonist that has been utilized in France for decades for the treatment of nausea and vomiting. Its pharmacologic profile is particularly attractive for gastroparesis because it is peripherally restricted, meaning it does not readily cross the blood-brain barrier. This characteristic theoretically eliminates the risk of extrapyramidal side effects. NG101, the mesylate salt of metopimazine, was developed to evaluate whether this established antiemetic could serve as a safe and effective oral therapy for the broader gastroparesis population.
Study Design and Methodology
The study was a Phase 2, multicenter, randomized, double-blind, placebo-controlled trial designed to assess the safety and efficacy of NG101. A total of 161 participants were randomized into four arms: placebo or NG101 at doses of 5 mg, 10 mg, or 20 mg, administered four times daily (QID).The study population was representative of the typical gastroparesis demographic, consisting of 45.3% diabetic gastroparesis (DG) and 54.7% idiopathic gastroparesis (IG) patients. The primary efficacy endpoint was the change from baseline in mean nausea severity, as recorded by the Diabetic and Idiopathic Gastroparesis Symptoms Daily Diary (DIGS-DD) during weeks 7 through 12. The DIGS-DD is a validated tool that captures symptom intensity on a 0–10 numeric rating scale.Secondary endpoints included the Patient Global Impression of Change (PGIC), which asked patients to rate their overall improvement in nausea and other symptoms on a 7-point balanced ordinal scale. Safety was monitored through adverse event reporting, laboratory assessments, and electrocardiograms (ECGs).
Key Findings: Reconciling Quantitative and Qualitative Data
Primary Efficacy Results
The trial results presented a nuanced picture of NG101’s efficacy. Regarding the primary endpoint—the reduction in mean nausea severity on the DIGS-DD—all NG101 treatment groups (5 mg, 10 mg, and 20 mg) showed a numerical decrease in nausea scores from baseline to the week 7–12 period. However, when compared to the placebo group, these improvements did not reach statistical significance. This phenomenon is common in gastroparesis trials, where high placebo response rates often mask the therapeutic effect of the investigational drug in daily diary assessments.
Global Improvements and Secondary Endpoints
In contrast to the daily diary data, the Patient Global Impression of Change (PGIC) for nausea yielded statistically significant results. During the 12-week treatment period, patients across all NG101 dose groups reported significantly greater overall improvement in their nausea compared to those receiving placebo. This discrepancy suggests that while daily rating scales may capture the granular fluctuations of symptoms, global assessment tools may better reflect the patient’s holistic perception of clinical benefit and quality of life improvement.
Subgroup Insights: Idiopathic vs. Diabetic Gastroparesis
A notable finding in the study was the divergent trend between gastroparesis etiologies. Patients with idiopathic gastroparesis appeared to respond more favorably to NG101 than those with diabetic gastroparesis. This difference may be attributed to the underlying pathophysiology; diabetic gastroparesis often involves more severe autonomic neuropathy and systemic complications that may complicate the response to a purely peripheral D2 antagonist.
Safety and Tolerability Profile
Safety is a critical benchmark for any new gastroparesis therapy. In this Phase 2 trial, NG101 demonstrated an excellent safety profile. The incidence of adverse events was comparable across the active treatment groups and the placebo group. Importantly, there were no reports of extrapyramidal symptoms or tardive dyskinesia, supporting the claim that NG101 is peripherally restricted. Furthermore, no clinically significant changes in QT intervals were observed, addressing the cardiac safety concerns that have hampered other agents in this class.
Expert Commentary: Interpreting the Results
The failure of NG101 to meet its primary endpoint in this Phase 2 trial highlights the ongoing challenges in gastroparesis research. The high placebo effect and the variability of daily symptom reporting frequently obscure the efficacy of prokinetic and antiemetic agents. However, the significant findings in the PGIC cannot be ignored. For clinicians, a patient’s global sense of improvement is often more relevant than a one-point shift on a daily diary.The trend toward greater efficacy in idiopathic gastroparesis is particularly intriguing. As the medical community moves toward precision medicine, identifying specific phenotypes—such as IG—that are more likely to respond to peripheral D2 antagonism could refine future trial designs and clinical applications. Mechanistically, the peripheral action of NG101 provides a much-needed safety margin, potentially allowing for long-term management without the fear of irreversible neurological damage.
Conclusion: The Path Forward
While the Phase 2 trial of NG101 did not achieve statistical significance for its primary endpoint of nausea severity reduction, the study provides valuable evidence of the drug’s safety and its positive impact on global patient well-being. The data suggest that NG101 remains a viable candidate for further investigation, particularly for the idiopathic gastroparesis subgroup. Future Phase 3 studies will likely need to optimize endpoint selection and perhaps focus on specific patient populations to fully elucidate the therapeutic potential of this peripherally restricted D2 antagonist.
Funding and Clinical Registration
This study was funded by Neurogastrx, Inc. The trial is registered at ClinicalTrials.gov under the identifier NCT04303195.
References
1. Loesch J, Hamza E, Pasricha PJ, et al. A Phase 2 Randomized, Double-Blind, Placebo-Controlled Study of the Safety and Efficacy of Metopimazine Mesylate (NG101) in Participants With Gastroparesis. Am J Gastroenterol. 2026;121(2):534-544. doi:10.14309/ajg.0000000000003534.
2. Camilleri M, Parkman HP, Shafi MA, et al. Clinical Guideline: Management of Gastroparesis. Am J Gastroenterol. 2013;108(1):18-37.
3. Parkman HP, Hallinan EK, Hasler WL, et al. Early Satiety and Postprandial Fullness in Gastroparesis. Dig Dis Sci. 2017;62(8):2043-2053.