Highlight
Cervical stromal invasion (CSI) has historically been considered a marker of poor prognosis in endometrial cancer, yet its independent impact remains debated. This multicenter study of over 7,000 patients reveals that after adjusting for confounding pathological features, CSI does not significantly influence progression-free survival (PFS) or overall survival (OS). The findings suggest that CSI often co-occurs with other aggressive features rather than acting as a standalone driver of mortality.
Background: The Evolution of Endometrial Cancer Staging
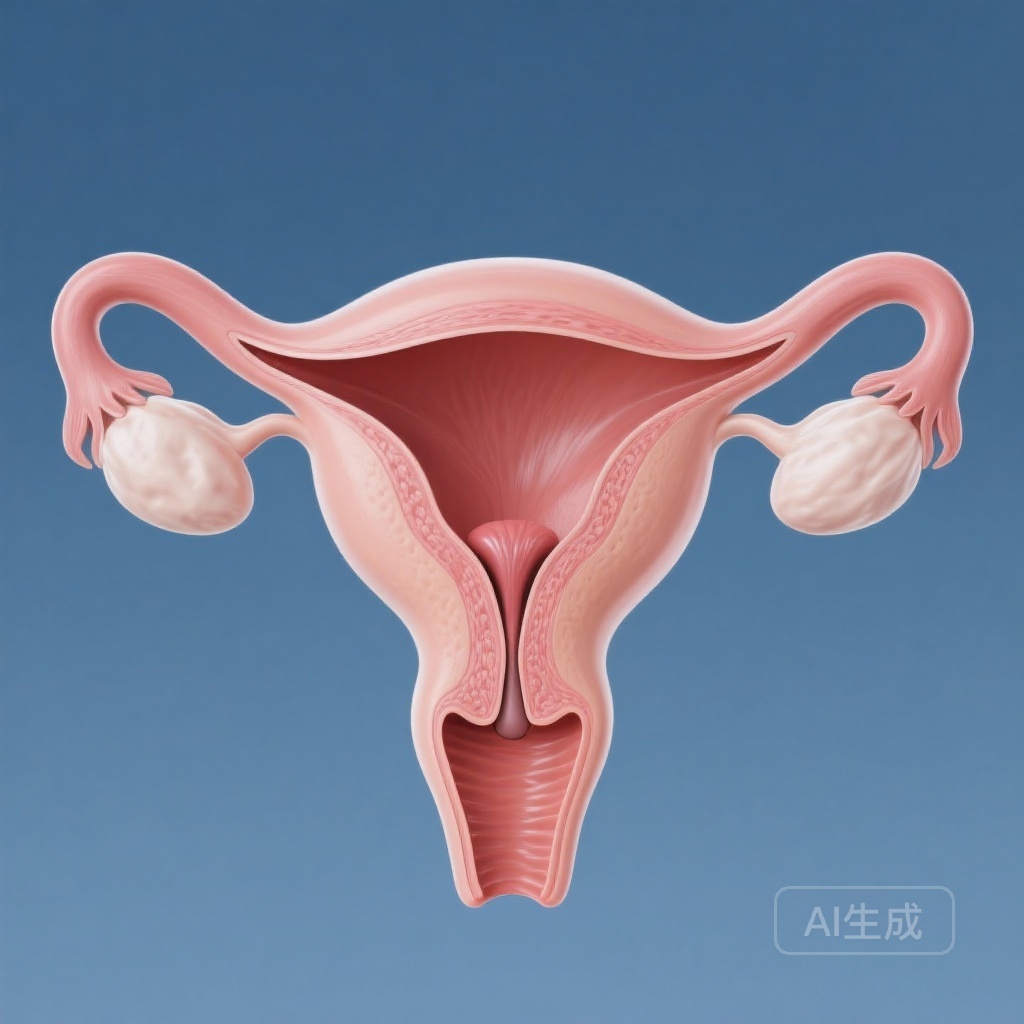
Endometrial cancer is the most common gynecological malignancy in developed nations. For decades, the International Federation of Gynecology and Obstetrics (FIGO) has refined the staging system to better reflect patient prognosis and guide adjuvant therapy. Under the FIGO 2009 staging system, the presence of cervical stromal invasion (CSI) upgrades a tumor from Stage I to Stage II. This transition typically triggers more aggressive management, including more radical surgery or intensive adjuvant radiation and chemotherapy.
However, clinical observation has long noted that tumors with CSI frequently exhibit other unfavorable characteristics, such as high-grade histology, deep myometrial invasion, or lymphovascular space invasion (LVSI). This confounding makes it difficult to ascertain whether the cervical involvement itself confers a worse prognosis or if it is merely a bystander in an overall more aggressive disease profile. Previous studies investigating this link have been hampered by small sample sizes and inconsistent methodologies, leading to a lack of consensus in the gynecologic oncology community.
Study Design and Methodology
To address this clinical uncertainty, a comprehensive multicenter retrospective study was conducted involving nine major regional medical institutions in China. The study analyzed data from 7,383 patients diagnosed with FIGO 2009 stage I-II endometrial cancer who underwent surgical staging between January 2000 and December 2019.
Patient Selection and Endpoints
The cohort was divided into two groups: those with histological evidence of cervical stromal invasion (n=524) and those without (n=6,859). The primary outcome was progression-free survival (PFS), defined as the time from surgery to the first evidence of disease recurrence or death. The secondary outcome was overall survival (OS).
Statistical Rigor
To ensure the findings were not skewed by the uneven distribution of high-risk factors, the researchers utilized two robust statistical approaches. First, a multivariable Cox proportional hazards regression model was applied to the entire cohort. Second, propensity score matching (PSM) was performed to create a balanced comparison. The variables matched included age at diagnosis, comorbidities (hypertension, diabetes), CA-125 levels, histological type, depth of myometrial invasion, LVSI, peritoneal cytology, surgical approach, type of hysterectomy, lymphadenectomy, and adjuvant therapy protocols.
Key Findings: CSI as a Non-Independent Variable
The results of this large-scale analysis provide a clear departure from traditional prognostic assumptions regarding cervical involvement.
Multivariable Analysis Results
In the initial analysis of the entire cohort, CSI appeared to be associated with worse outcomes in a univariate model. However, once the model was adjusted for other prognostic factors, the association vanished. The adjusted hazard ratio (aHR) for progression-free survival was 1.31 (95% CI, 0.94-1.81; P=.106). Similarly, for overall survival, the aHR was 1.33 (95% CI, 0.88-2.00; P=.171). Both results failed to reach statistical significance, indicating that CSI does not independently increase the risk of recurrence or death.
Propensity Score-Matched (PSM) Cohort
After matching patients to ensure identical baseline characteristics, the survival curves for both groups were nearly identical. The 5-year PFS for patients with CSI was 92.3%, compared to 93.7% for those without (P=.493). The 5-year OS rates were 95.0% and 95.7%, respectively (P=.791). This lack of difference persisted even when the researchers conducted subgroup analyses based on histological type (e.g., endometrioid vs. non-endometrioid) and the type of adjuvant therapy received.
Expert Commentary and Clinical Implications
The findings of this study by Li et al. are particularly timely given the recent updates to FIGO staging in 2023, which place a heavier emphasis on molecular classification and other pathological markers. The data suggests that the anatomical spread to the cervical stroma may be less relevant than the underlying biological aggressiveness of the tumor.
Biological Plausibility
One potential explanation for these findings is that the cervical stroma does not provide a significantly different microenvironment for tumor growth compared to the uterine corpus. If a tumor is biologically predisposed to metastasize, it will likely do so regardless of whether it has crossed the internal os into the cervix. Therefore, if the tumor is surgically removed with clear margins and appropriate adjuvant therapy is administered based on other risk factors (like grade and LVSI), the specific presence of CSI may not add additional risk.
Impact on Treatment De-escalation
For clinicians, these results raise important questions about the necessity of radical hysterectomy or intensified radiation for Stage II patients whose only high-risk feature is CSI. If CSI is not an independent driver of poor outcomes, some patients might be over-treated, leading to unnecessary surgical morbidity or long-term side effects from radiation without a commensurate survival benefit.
Study Limitations
While the study is robust due to its multicenter nature and large sample size, it is not without limitations. As a retrospective study, it is subject to inherent selection biases, although the use of PSM mitigates this. Furthermore, the study spans two decades, during which surgical techniques (such as the rise of minimally invasive surgery) and adjuvant therapy standards evolved significantly. Finally, the study did not incorporate the latest molecular profiling (e.g., POLE mutation, MSI status), which is now considered the gold standard for endometrial cancer risk stratification.
Summary and Conclusion
In conclusion, this multicenter retrospective study demonstrates that cervical stromal invasion is not an independent prognostic factor for PFS or OS in women with early-stage endometrial cancer. While CSI is often found in conjunction with other adverse features, it does not appear to dictate survival outcomes on its own. These findings support a more nuanced approach to staging and treatment planning, where clinical decisions are driven by a composite of pathological and molecular markers rather than anatomical cervical involvement alone.
References
Li Z, Yang Y, Fang Y, et al. The prognostic and clinical significance of cervical stromal invasion in endometrial cancer: a multicenter retrospective study. Am J Obstet Gynecol. 2025;232(1):S0002-9378(25)00941-X. doi:10.1016/j.ajog.2025.12.044.