Highlights
- The Minima Stent System achieved a 97.6% procedural success rate in treating pulmonary artery stenosis (PAS) and coarctation of the aorta (CoA) in infants and young children.
- The trial demonstrated a median vessel diameter increase of 131% and a complete resolution of median pressure gradients (25 to 0 mm Hg) in coarctation patients.
- The device is specifically engineered to accommodate somatic growth, with 31% of patients undergoing successful planned re-expansion during follow-up.
- Safety outcomes remained robust with no device-related serious adverse events or explants reported through the six-month primary endpoint.
Background: Addressing the Therapeutic Gap in Pediatric Interventional Cardiology
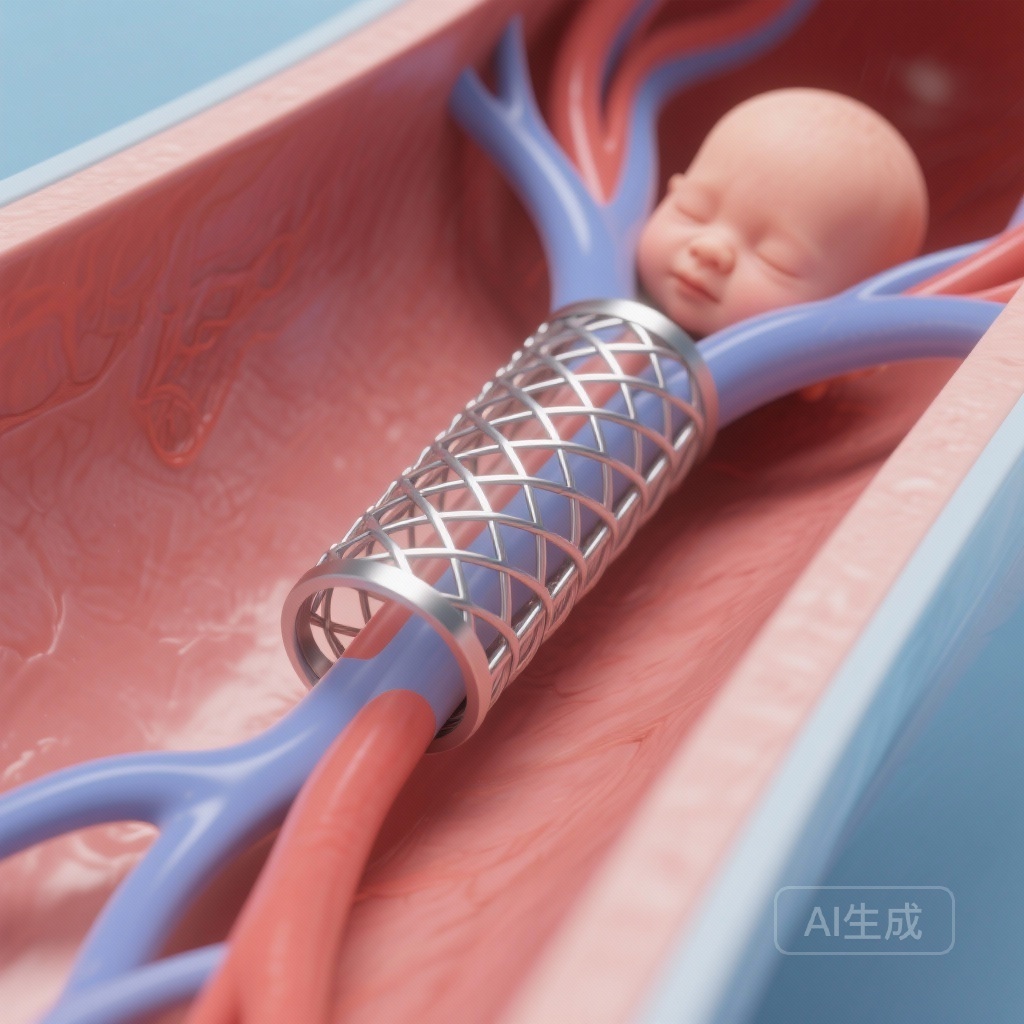
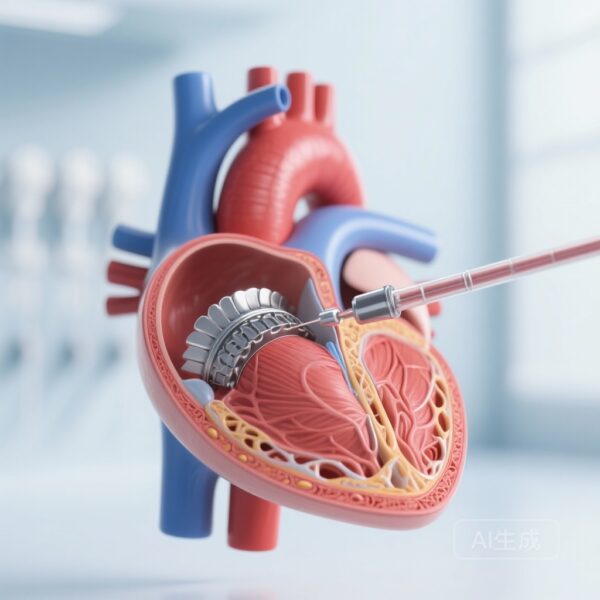
Vascular stenosis, specifically pulmonary artery stenosis (PAS) and coarctation of the aorta (CoA), remains a significant challenge in neonatal and infant cardiac care. While transcatheter stent implantation is a well-established therapy in older children and adults, its application in the smallest patients has historically been hindered by the lack of dedicated technology. Traditional stents are often designed for adult anatomy, lacking the flexibility, low profile, and, most importantly, the growth potential required for a developing child.
Infants with vascular stenosis frequently require surgical intervention because existing stents cannot be expanded sufficiently to match their future adult vessel size. The Minima Stent System (Renata Medical) was developed as a bespoke solution to this problem. It is the first stent system specifically designed, tested, and Food and Drug Administration (FDA)-approved for use in neonates, infants, and small children. The pivotal trial sought to provide the high-quality clinical evidence necessary to validate this breakthrough technology as a safe and effective alternative to surgery or off-label use of adult-sized devices.
Study Design and Patient Population
The study was a multicenter, single-arm, prospective, nonrandomized pivotal trial. It enrolled 42 patients across several high-volume pediatric cardiac centers. The cohort was diverse in its clinical presentation, including 21 patients with PAS, 15 with recurrent CoA, and 6 with native CoA. The median age at the time of implantation was 9 months, with a wide range spanning from 0.4 months (neonate) to 112 months. The median weight was 7.8 kg, with the smallest patient weighing only 3.4 kg.
The primary endpoints were meticulously selected to assess both safety and efficacy. These included the successful relief of stenosis, freedom from device-related serious adverse events (SAEs) or surgical intervention through 6 months, and the maintenance of vessel lumen diameter as confirmed by computed tomography (CT) or catheter angiography at the 6-month follow-up mark.
Key Findings: Efficacy and Hemodynamic Impact
The trial reported a high level of technical and clinical success. Implantation was successful in 41 out of 42 patients (97.6%). The hemodynamic improvements were statistically and clinically significant. Among patients with coarctation of the aorta, the median pressure gradient was reduced from 25 mm Hg (range 0–63) to 0 mm Hg (range 0–6; P < 0.001). This complete resolution of the gradient in most patients highlights the stent's immediate impact on cardiovascular physiology.
Vessel diameter measurements further supported the stent’s efficacy. There was a median increase in minimal vessel diameter of 131%, with some patients experiencing an increase as high as 483%. At the six-month follow-up, luminal patency was remarkably well-preserved, maintaining 89% of the initial implant diameter. This stability is crucial, as it suggests the stent does not suffer from significant early recoil or excessive neointimal hyperplasia that would necessitate premature reintervention.
Safety Profile and Procedural Considerations
The safety data from the trial were encouraging, though they highlighted the inherent risks of intervention in very small patients. There were no device-related SAEs, deaths, or surgical explants during the primary six-month study period. However, procedural complications did occur. Two acute stent embolizations were noted in PAS patients; both stents were safely secured in the contralateral pulmonary artery, and one patient was successfully treated with an additional Minima stent.
A notable finding was the occurrence of transient femoral artery thrombosis in seven patients. Significantly, all of these patients weighed less than 6 kg. This underlines the technical challenges of vascular access in neonates and very small infants, though the investigators noted that these events were transient and did not lead to long-term sequelae. The low profile of the Minima delivery system is designed to mitigate these risks, but vascular complications remain a focal point for procedural refinement in the low-birth-weight population.
Accommodating Somatic Growth: The Role of Planned Expansion
The most innovative feature of the Minima Stent is its capacity for re-expansion to accommodate the child’s growth. During a median follow-up of 596 days, 13 patients (31%)—comprising 7 with CoA and 6 with PAS—underwent planned stent expansion. These procedures were performed to ensure the stent diameter kept pace with the patient’s increasing vessel size. All re-expansions were completed without complications, demonstrating that the stent can be safely manipulated after the initial implant. This capability potentially reduces the lifetime surgical burden for these patients, as the stent can grow with them until they reach a size where a permanent, adult-sized stent can be placed if necessary.
Expert Commentary
The results of the Minima pivotal trial represent a landmark moment in pediatric interventional cardiology. For years, clinicians have had to rely on off-label use of biliary or small vascular stents that were never intended to be expanded to adult diameters. The Minima stent changes this paradigm by providing a dedicated platform that balances the need for initial low-profile delivery with the necessity of future large-diameter expansion.
While the study is limited by its single-arm design and relatively small sample size, the prospective nature and multicenter involvement provide robust data that are highly generalizable to specialized pediatric cardiac programs. The high rate of femoral thrombosis in infants under 6 kg suggests that while the stent itself is optimized, the delivery techniques and periprocedural anticoagulation protocols for the smallest neonates may still require further optimization. Nevertheless, the ability to avoid open-heart surgery in an infant by using a growth-accommodating stent is a significant advancement in patient-centered care.
Conclusion
The Minima Stent System is a safe and effective tool for treating vascular stenosis in the most vulnerable pediatric populations. By providing significant hemodynamic relief and maintaining luminal patency while allowing for safe re-expansion, the system addresses the critical problem of somatic growth in pediatric cardiology. As long-term follow-up continues, the Minima stent is poised to become the standard of care for neonatal and infant PAS and CoA, offering a bridge to maturity that minimizes the need for early surgical intervention.
Funding and Registration
This study was supported by Renata Medical. ClinicalTrials.gov Identifier: NCT05086016.
References
Sullivan PM, Zahn EM, Sathanandam S, Morray B, Shahanavaz S, Salavitabar A, Armstrong AK, Porras D, Berman DP. Multicenter Pivotal Trial of the Minima Stent for Vascular Stenosis in Infants and Young Children. Circ Cardiovasc Interv. 2025 Dec;18(12):e015618. doi: 10.1161/CIRCINTERVENTIONS.125.015618. Epub 2025 Oct 10. PMID: 41070410.