Highlight
- The ARCADIA-MRI ancillary study found no statistically significant difference in incident intracranial hemorrhages (>10 mm) between patients treated with apixaban and those treated with aspirin.
- The rates of incident cerebral microbleeds and cortical superficial siderosis (CSS) were comparable between the two treatment arms over a median follow-up of 27 months.
- These findings suggest that for patients with atrial cardiopathy and cryptogenic stroke, the use of an oral anticoagulant (apixaban) does not increase the burden of subclinical or overt hemorrhagic lesions compared to antiplatelet therapy (aspirin).
Background: The Challenge of Atrial Cardiopathy and Cryptogenic Stroke
Cryptogenic stroke, often classified under the umbrella of Embolic Stroke of Undetermined Source (ESUS), remains a significant diagnostic and therapeutic challenge in vascular neurology. Recent research has shifted focus from identifying overt atrial fibrillation to recognizing ‘atrial cardiopathy’—a structural, functional, or electrical disorder of the left atrium that may predispose patients to thromboembolism even in the absence of documented arrhythmia.
The ARCADIA (Atrial Cardiopathy and Antithrombotic Drugs in Prevention After Cryptogenic Stroke) trial was designed to determine if apixaban, a direct oral anticoagulant (DOAC), is superior to aspirin in preventing recurrent stroke in this population. While the primary ARCADIA trial did not demonstrate a significant difference in recurrent stroke rates between the two groups, the ARCADIA-MRI ancillary study provided a unique opportunity to examine the subclinical effects of these drugs on brain tissue, specifically regarding covert infarcts and hemorrhagic lesions.
A critical concern when prescribing anticoagulation over antiplatelet therapy is the potential for increased intracranial bleeding. This study specifically aimed to quantify this risk using sensitive neuroimaging markers, providing clinicians with essential safety data regarding the long-term use of apixaban in patients with stroke and atrial cardiopathy.
Study Design and Methodology
The ARCADIA-MRI study was a prespecified, exploratory ancillary study conducted at select sites within the larger ARCADIA randomized trial. The study population consisted of patients who had experienced a cryptogenic stroke and met specific criteria for atrial cardiopathy, defined by at least one of the following: a P-wave terminal force in lead V1 (PTFV1) > 5000 μV·ms on ECG, N-terminal pro-brain natriuretic peptide (NT-proBNP) > 250 pg/mL, or a left atrial diameter index ≥ 2.0 cm/m² on echocardiography.
Patients were randomized 1:1 to receive either apixaban (5 mg or 2.5 mg twice daily, based on standard dosing criteria) or aspirin (81 mg daily). Inclusion in the MRI substudy required eligibility for cognitive testing and the absence of MRI contraindications. Baseline and follow-up MRI scans were performed, with follow-up durations ranging from 4 months to 5.3 years, maintaining a median follow-up of 27 months.
Radiologic Endpoints
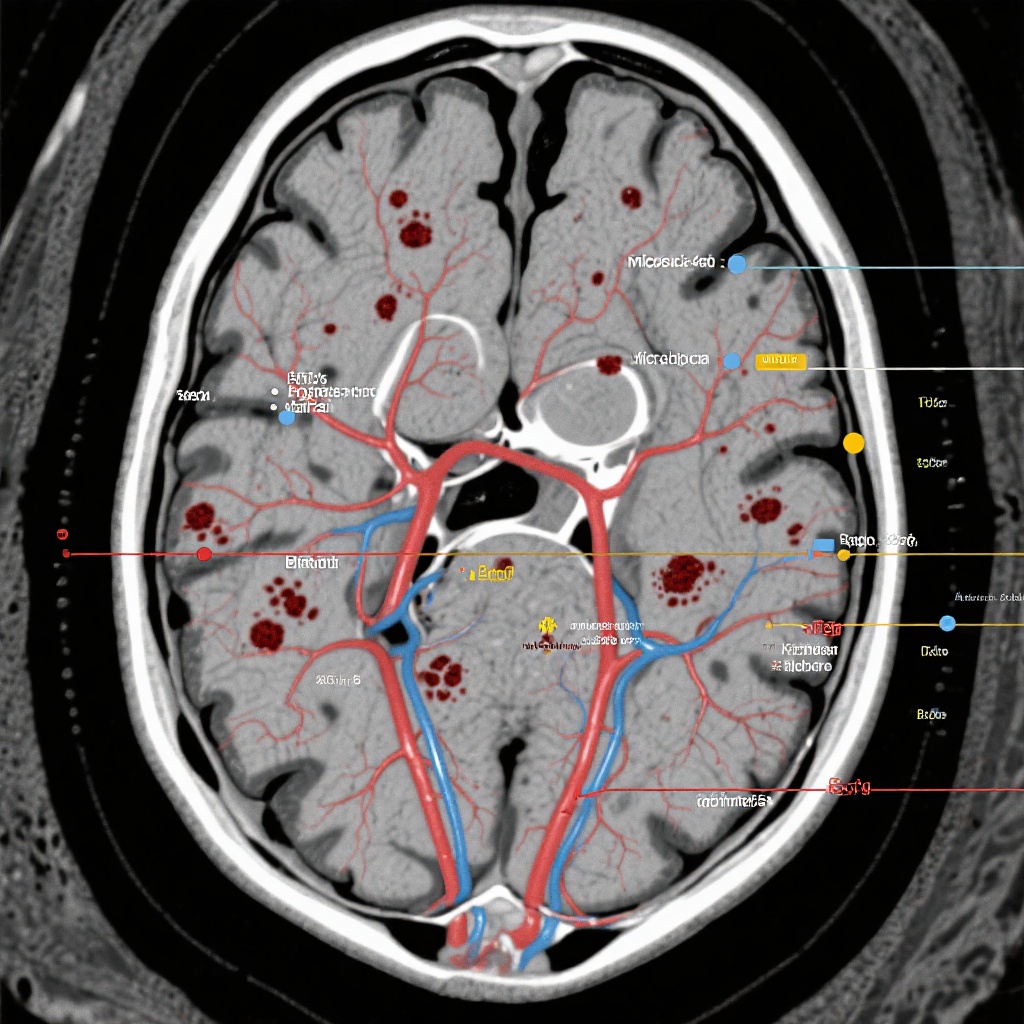
Two experienced raters, who were entirely blinded to the treatment assignments, independently evaluated the MRI scans. The primary radiologic end points for this specific analysis were:
- Incident Intracranial Hemorrhage (ICH): Defined as a bleeding event greater than 10 mm in diameter.
- Cerebral Microbleeds (CMBs): Defined as small, rounded areas of signal void on susceptibility-weighted imaging (SWI) or T2*-weighted gradient-recalled echo (GRE) sequences, measuring 10 mm or less.
- Cortical Superficial Siderosis (CSS): Characterized by linear residues of blood products in the subarachnoid space or superficial layers of the cerebral cortex.
Key Findings: A Comparative Analysis of Hemorrhagic Events
The analysis included 174 patients who completed both baseline and follow-up MRI scans (79 in the apixaban group and 95 in the aspirin group). At baseline, the demographics and the prevalence of preexisting MRI markers were well-balanced between the two treatment cohorts. This provided a stable foundation for comparing the incidence of new lesions during the follow-up period.
Incident Bleeding Events
The results indicated no statistically significant differences in the development of new hemorrhagic lesions between the apixaban and aspirin groups. The specific findings were as follows:
1. Intracranial Hemorrhage (>10 mm)
Incident ICH occurred in 5.1% of patients in the apixaban group compared with 6.4% in the aspirin group. The slight numerical difference favored apixaban, though it did not reach statistical significance (P > .05).
2. Cerebral Microbleeds (≤10 mm)
The development of new microbleeds was observed in 7.8% of the apixaban group and 10.8% of the aspirin group. Again, there was no evidence that anticoagulation with apixaban led to a higher burden of small-vessel hemorrhagic markers compared to standard antiplatelet therapy.
3. Cortical Superficial Siderosis (CSS)
Incident CSS, often a marker of cerebral amyloid angiopathy or previous subarachnoid hemorrhage, was found in 7.7% of the apixaban group and 12.9% of the aspirin group. This finding is particularly noteworthy as CSS is a strong predictor of future symptomatic ICH, and the lack of an increase in the apixaban group supports its safety profile.
Overall, the exploratory analysis suggests that apixaban is not associated with an increased risk of radiologic bleeding markers when compared to aspirin in this specific high-risk stroke population.
Expert Commentary and Clinical Implications
The ARCADIA-MRI findings contribute significantly to our understanding of the safety of DOACs in patients with cryptogenic stroke. Historically, clinicians have been cautious about using anticoagulants in patients with high burdens of cerebral microbleeds or superficial siderosis due to the perceived risk of catastrophic intracranial hemorrhage. The data from this ancillary study provide a degree of reassurance.
Mechanistic Insights
The comparable rates of microbleeds and CSS between apixaban and aspirin may be attributed to the specific pharmacological profile of Factor Xa inhibitors. Unlike warfarin, which inhibits multiple clotting factors and can lead to more profound alterations in the coagulation cascade, apixaban provides a more targeted inhibition that may preserve some level of hemostatic response in the cerebral microvasculature. Furthermore, the findings suggest that the underlying small vessel disease (SVD) progression, which drives these hemorrhagic markers, may be relatively independent of the choice of antithrombotic agent within the limits of this study’s duration.
Comparison with Primary ARCADIA Results
While the primary ARCADIA trial did not show apixaban to be superior to aspirin for preventing recurrent clinical stroke, the MRI substudy previously reported a lower risk of incident nonlacunar covert infarcts in the apixaban group. When combined with the current findings showing no increase in bleeding, it highlights a nuanced benefit: while clinical stroke rates were similar, apixaban may offer better protection against subclinical embolic events without the penalty of increased subclinical bleeding.
Study Limitations
As an exploratory analysis, several limitations must be considered. First, the sample size of 174 patients is relatively small for detecting rare events like symptomatic ICH. Second, the duration of follow-up, while significant at a median of 27 months, may not capture the very long-term cumulative effects of antithrombotic therapy on microvascular integrity. Finally, the study was not powered to detect small differences in bleeding rates, and the results should be interpreted as hypothesis-generating rather than definitive.
Conclusion
In conclusion, the ARCADIA-MRI ancillary study demonstrates that in patients with cryptogenic stroke and evidence of atrial cardiopathy, the use of apixaban does not result in a higher incidence of intracranial hemorrhage, cerebral microbleeds, or cortical superficial siderosis compared to aspirin. These findings support the safety of apixaban in this population from a neuroimaging perspective. While the primary trial did not support a change in the standard of care for all ESUS patients, these sub-study results provide critical safety data that may inform individualized treatment decisions, particularly in patients where the risk of covert infarction is high and the concern for hemorrhagic transformation is paramount.
Funding and ClinicalTrials.gov
The ARCADIA trial and its ancillary studies were supported by grants from the National Institute of Neurological Disorders and Stroke (NINDS). ClinicalTrials.gov Identifier: NCT03192280.
References
- Chen H, Lansberg M, Zhu G, et al. MRI Findings of Intracranial Hemorrhages in ARCADIA-MRI: An Ancillary Study to the ARCADIA Trial. AJNR Am J Neuroradiol. 2026;47(2):322-328. doi:10.3174/ajnr.A8955.
- Kamel H, Longstreth WT Jr, Tirschwell DL, et al. The Atrial Cardiopathy and Antithrombotic Drugs in Prevention After Cryptogenic Stroke (ARCADIA) Trial: Methods and Baseline Characteristics. J Stroke Cerebrovasc Dis. 2019;28(11):104333.
- Healey JS, Gladston DJ, Crystal E, et al. Atrial Fibrillation in Patients with Cryptogenic Stroke. N Engl J Med. 2014;370:2478-2486.