Posted inCardiology Internal Medicine news
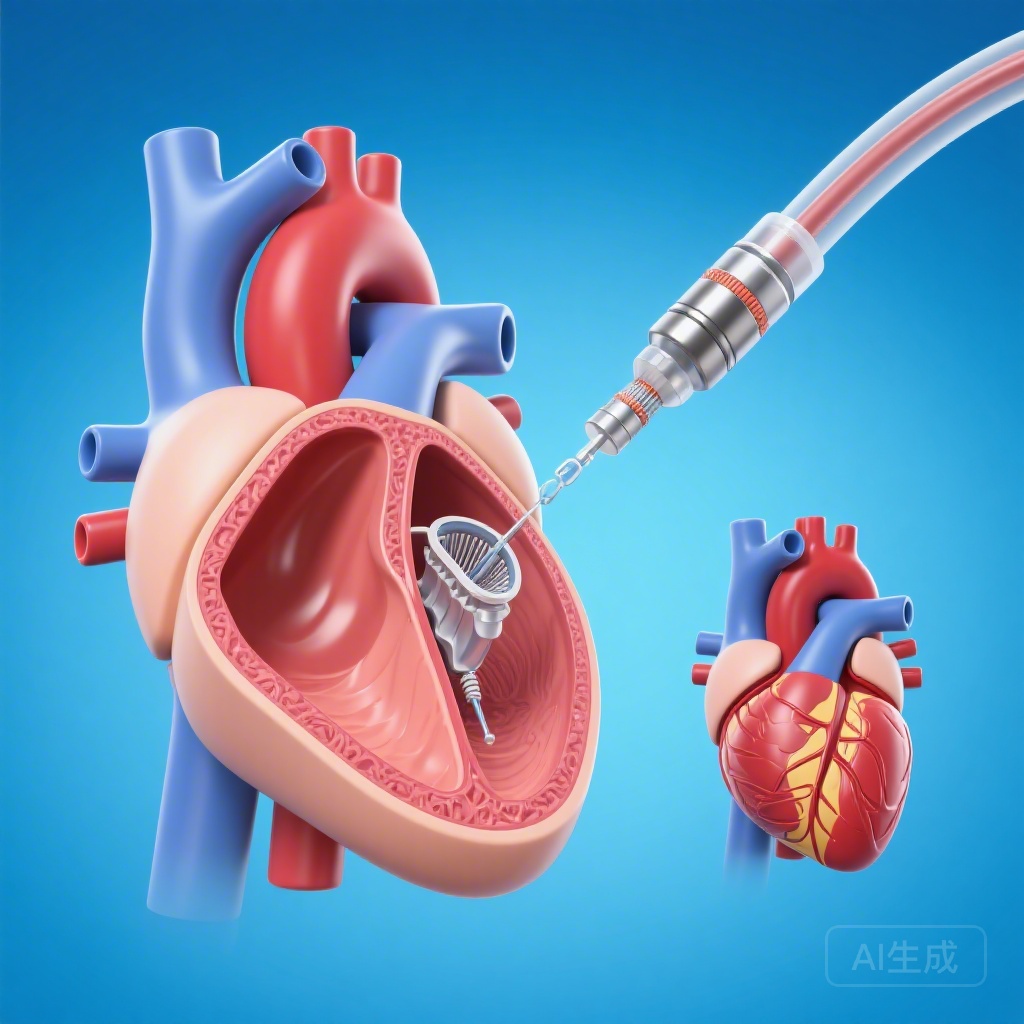
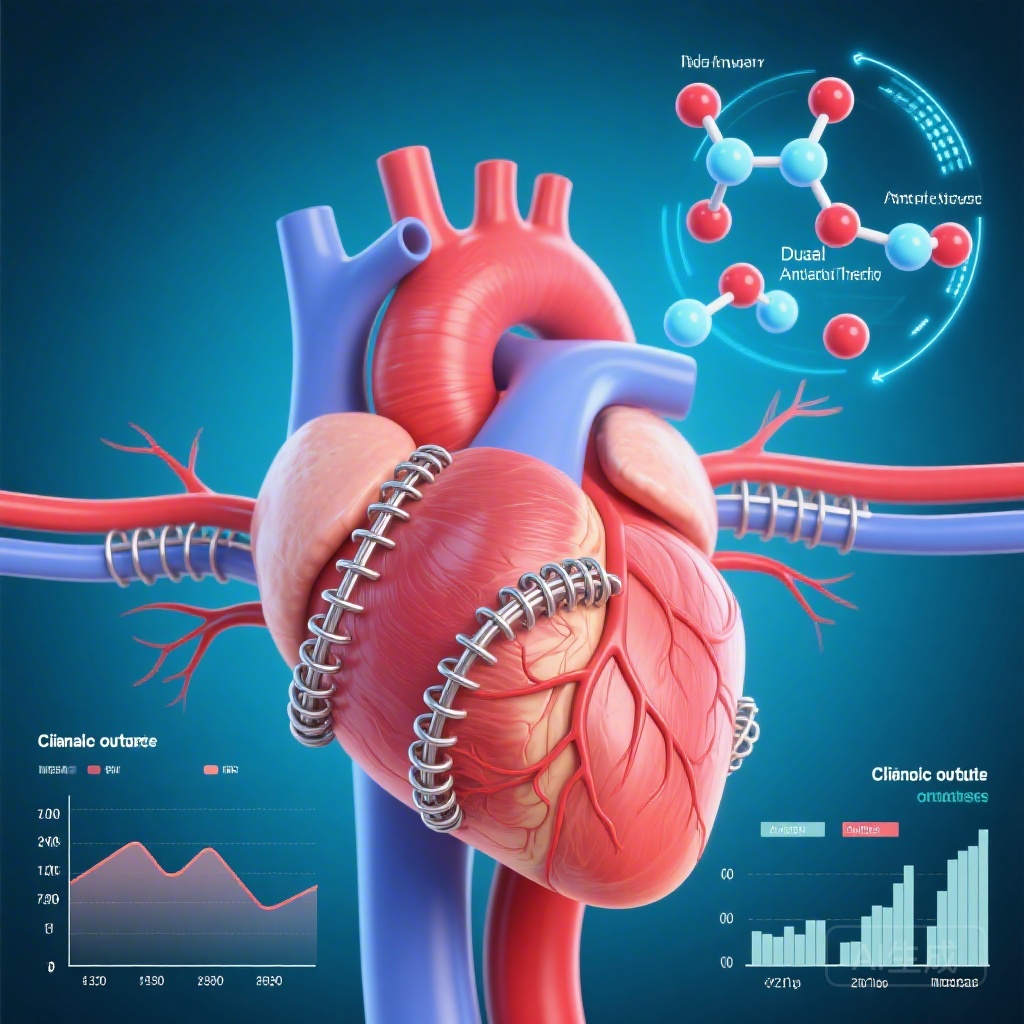
Pharmacist-Led Patient Self-Testing Superior to Usual Care for Warfarin Management in Mechanical Heart Valve Patients: Evidence from a Multicentre RCT in China
A multicentre RCT in China found that pharmacist-led patient self-testing (PST) significantly improves time in therapeutic range and reduces major bleeding and thromboembolism in patients with mechanical heart valves compared to traditional outpatient clinic care.