Highlights
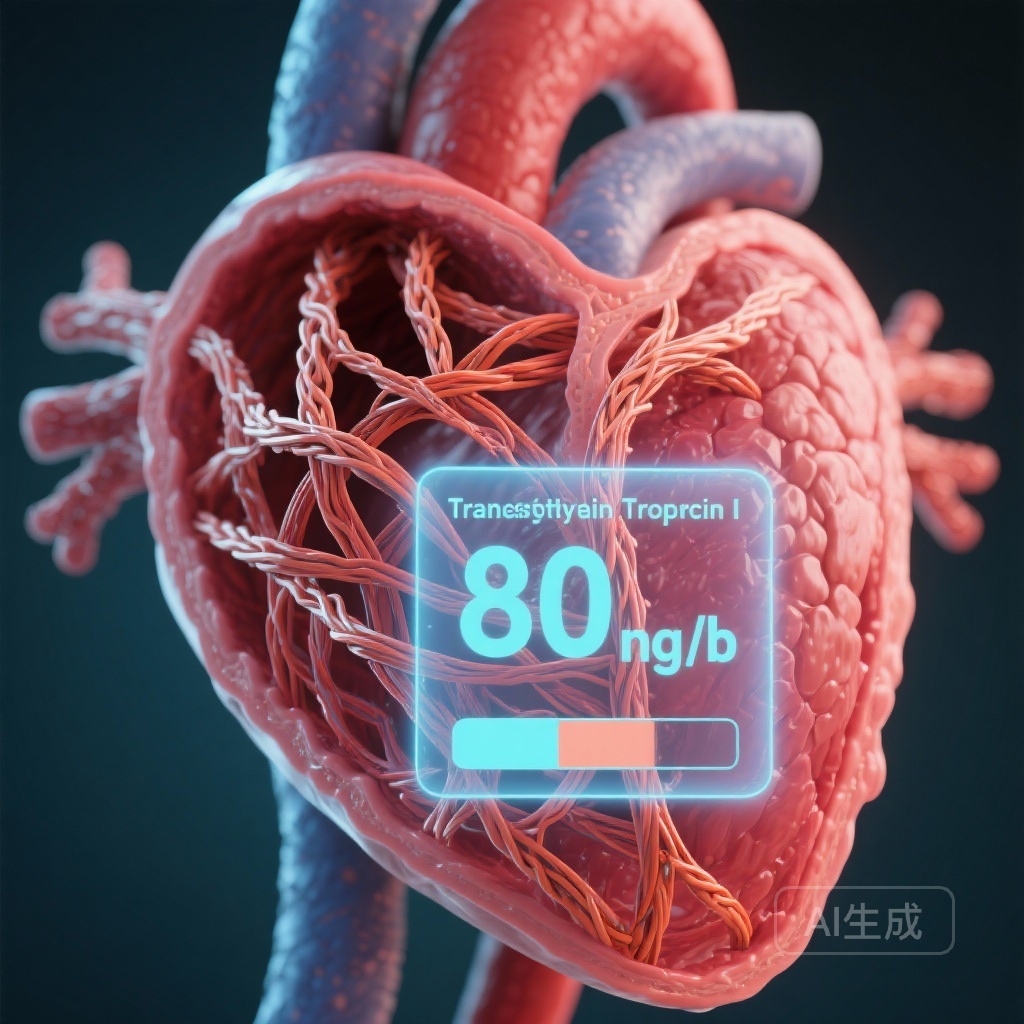
1. High-sensitivity cardiac troponin I (hs-cTnI) is established as an independent predictor of all-cause mortality in patients with wild-type transthyretin amyloid cardiomyopathy (ATTRwt-CM).
2. A standardized clinical threshold of 80 ng/L for hs-cTnI was identified and validated across three major assay platforms (Abbott, Beckman Coulter, and Siemens), simplifying risk assessment in clinical practice.
3. Combining hs-cTnI (>80 ng/L) with natriuretic peptides (NT-proBNP >3000 ng/L or BNP >250 ng/L) creates a high-performance, two-variable staging system that effectively discriminates survival outcomes across three distinct risk groups.
Disease Burden and Clinical Context
Wild-type transthyretin amyloid cardiomyopathy (ATTRwt-CM) has transitioned from being considered a rare condition to a frequently recognized cause of heart failure with preserved ejection fraction (HFpEF), particularly in the elderly population. The pathophysiology involves the dissociation of the transthyretin tetramer into unstable monomers, which misfold and aggregate into amyloid fibrils that deposit in the myocardial extracellular space. This process leads to progressive restrictive cardiomyopathy, conduction disturbances, and eventually, death.
Accurate risk stratification is critical for clinical decision-making, particularly with the advent of expensive disease-modifying therapies such as TTR stabilizers. While the Mayo Clinic 2012 staging system—incorporating cardiac troponin T (cTnT) and N-terminal pro-B-type natriuretic peptide (NT-proBNP)—has been the gold standard, the clinical laboratory landscape has shifted toward high-sensitivity cardiac troponin I (hs-cTnI). However, the multiplicity of hs-cTnI assays and a lack of standardized prognostic thresholds have limited its integration into formal staging systems for ATTRwt-CM. This study addresses this gap by seeking a universal threshold applicable across different manufacturers.
Study Design and Methodology
This observational multicenter study utilized cohorts of stable patients diagnosed with ATTRwt-CM. The research was structured into a testing phase and a validation phase. The testing cohorts included 136 patients evaluated with the Abbott Architect Stat hs-cTnI assay and 98 patients evaluated with the Beckman Coulter Access hs-cTnI assay. The validation cohort consisted of 345 patients evaluated with the Siemens Centaur XPT hs-cTnI assay.
The primary endpoint was all-cause mortality. Researchers employed natural log-transformation of hs-cTnI levels to assess their independent predictive value through Cox proportional hazards models, adjusted for age and sex. The optimal prognostic threshold for 18-month mortality was determined using the Youden index and subsequently rounded for clinical utility. Finally, the researchers integrated this threshold into a two-variable staging system modeled after the Mayo Clinic framework, substituting hs-cTnI for traditional troponin measures.
Key Findings: hs-cTnI as a Potent Prognostic Marker
Independent Predictive Value
In the Abbott cohort, with a median follow-up of 22 months, 23% of patients died. Natural log-transformed hs-cTnI was a significant independent predictor of mortality, yielding an age- and sex-adjusted hazard ratio (HR) of 1.62 (95% CI, 1.11–2.35; P=0.012). The Beckman cohort showed even more pronounced results over a 19-month median follow-up, with a 16% mortality rate and an adjusted HR of 2.47 (95% CI, 1.48–4.14; P<0.001).
The Universal 80 ng/L Threshold
One of the study’s most significant contributions is the identification of a unified threshold. By analyzing the combined Abbott and Beckman cohorts (n=234), the researchers identified 81 ng/L as the optimal cutoff for 18-month mortality. For ease of clinical application, this was rounded to 80 ng/L. This threshold proved robust, effectively separating patients into high- and low-risk categories regardless of the specific assay used.
Validation of the Staging System
The proposed staging system utilizes two variables: hs-cTnI (>80 ng/L) and natriuretic peptides (NT-proBNP >3000 ng/L or BNP >250 ng/L). Patients are categorized into three stages:
– Stage I: Both markers below the threshold.
– Stage II: One marker above the threshold.
– Stage III: Both markers above the threshold.
When applied to the independent validation cohort (Siemens assay, n=345), where 34% of patients died over a 32-month median follow-up, the staging system maintained its high discriminative power. The survival curves for the three groups showed significant separation (P<0.001), confirming that the 80 ng/L hs-cTnI threshold is globally applicable for risk stratification in ATTRwt-CM.
Expert Commentary: Mechanistic Insights and Clinical Utility
The elevation of cardiac troponins in amyloidosis is not typically due to acute coronary syndromes but rather reflects chronic, ongoing cardiomyocyte injury. This injury is likely mediated by the direct toxic effects of amyloid oligomers and the mechanical stress exerted by extracellular fibril deposition. The finding that hs-cTnI serves as a better or equal predictor compared to older assays is consistent with its ability to detect minute levels of myocardial damage.
From a clinical perspective, the transition to a two-variable system (hs-cTnI and NT-proBNP) simplifies the diagnostic workflow. Clinicians have often struggled with the variability between troponin I and T; this study provides a clear, evidence-based target for troponin I. Furthermore, the use of 80 ng/L—a value significantly higher than the 99th percentile upper reference limit for the general population—highlights the unique baseline elevation seen in amyloid patients and prevents over-diagnosis of ‘acute’ events in stable patients.
However, some limitations must be considered. While the study included multiple assays, the cohorts were primarily composed of stable patients. The performance of these thresholds in patients with significant comorbidities, such as advanced chronic kidney disease (CKD), which can independently elevate troponin levels, requires further investigation. Additionally, while all-cause mortality is a robust endpoint, the impact of these thresholds on predicting heart failure hospitalizations or quality-of-life deterioration remains to be fully elucidated.
Conclusion
The study by De Michieli et al. provides a critical update to the prognostic toolkit for wild-type transthyretin amyloid cardiomyopathy. By establishing 80 ng/L as a universal hs-cTnI threshold, the research enables a standardized approach to risk stratification that transcends assay-specific variations. Integrating this threshold into a two-variable staging system with natriuretic peptides offers clinicians a reliable, accessible method to identify high-risk patients who may require more intensive monitoring or earlier therapeutic intervention. As ATTRwt-CM continues to be diagnosed with increasing frequency, such standardized metrics will be essential for optimizing patient management and clinical trial design.
References
De Michieli L, Sinigiani G, Guida G, et al. High-Sensitivity Cardiac Troponin I for Risk Stratification in Wild-Type Transthyretin Amyloid Cardiomyopathy. Circ Heart Fail. 2025 Aug;18(8):e012816. doi: 10.1161/CIRCHEARTFAILURE.125.012816. Epub 2025 May 15. PMID: 40371473.