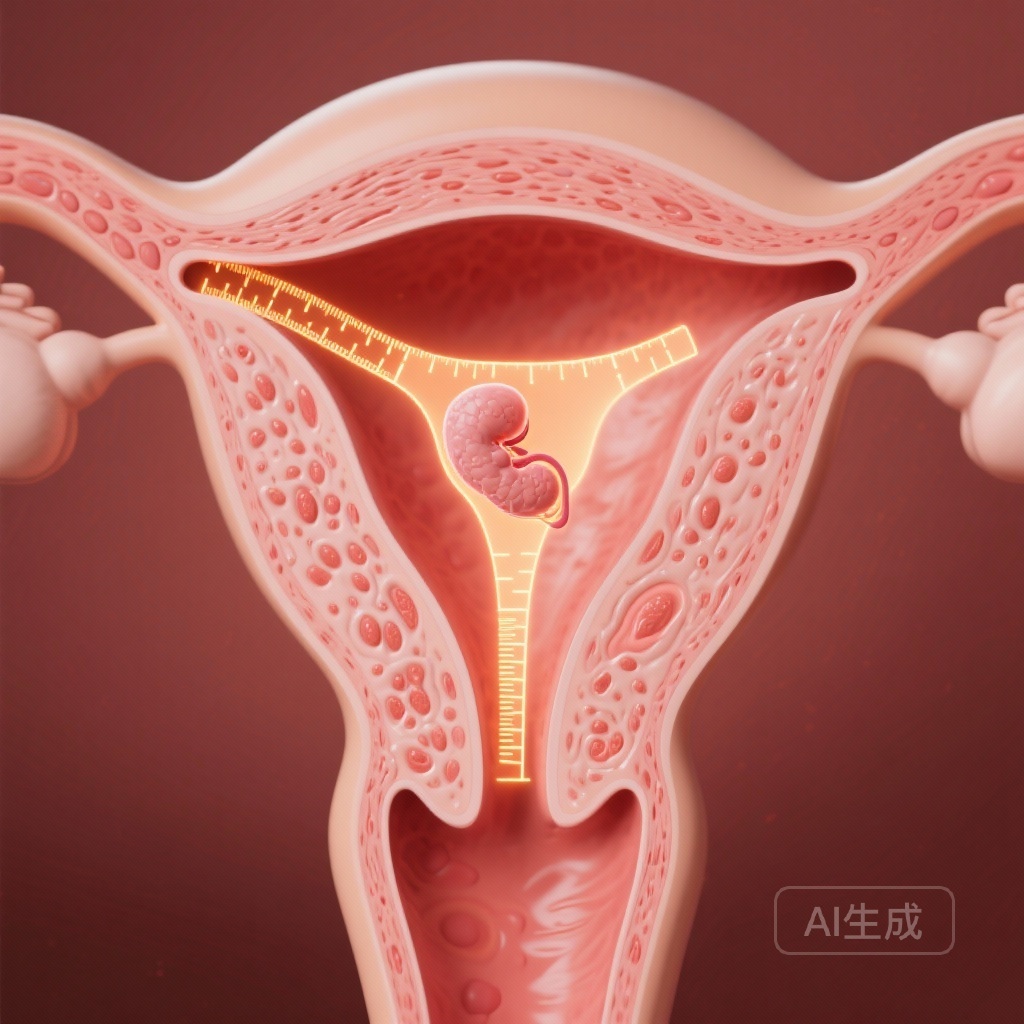
Introduction: The Persistent Dilemma of the Thin Endometrium
The pursuit of optimizing success in assisted reproductive technology (ART) has led to a granular focus on the uterine environment. Among the various biomarkers of endometrial receptivity, endometrial thickness (ET) remains one of the most debated and frequently measured parameters in clinical practice. For decades, clinicians have grappled with the ‘thin endometrium’—a condition often perceived as a major impediment to successful implantation and live birth. However, despite its ubiquitous use, the evidence defining a definitive threshold for ET has been inconsistent, often confounded by variations in embryo quality and transfer protocols.
The Shift Toward Euploid Transfers
The advent of preimplantation genetic testing for aneuploidy (PGT-A) has revolutionized the field by allowing for the selection of euploid embryos, thereby theoretically removing embryo quality as a primary variable for failure. This shift provides a unique opportunity to isolate the impact of the endometrium on reproductive outcomes. A new multicenter study by Genovese et al., recently published in Human Reproduction, seeks to provide clarity on this issue by analyzing over 30,000 euploid single embryo transfers (SET).
Study Design and Methodology
This international, retrospective cohort study is one of the largest of its kind, encompassing data from 25 IVF centers across three countries (USA, Spain, and the UAE) between 2017 and 2022. The primary objective was to determine if ET impacts the live birth rate (LBR) in patients undergoing a single euploid frozen embryo transfer (FET).
Population and Protocols
The study included a total of 30,676 cycles. All FET cycles involved a single euploid blastocyst created with autologous oocytes. The endometrial preparation protocols were categorized into three main groups: programmed cycles (using exogenous estrogen and progesterone), natural cycles (NC), and modified natural cycles (mNC, which typically include a trigger for ovulation).
Analytical Approach
The primary outcome was LBR stratified by ET and cycle type. To ensure a robust analysis, the researchers utilized conditional density plots (CDPs) to visualize the association between ET measurements and LBR. Multivariable logistic regression was employed to adjust for potential confounders, and receiver operating characteristics (ROC) curves were generated to evaluate the prognostic value of ET as a standalone predictor for pregnancy success.
Key Findings: A Protocol-Dependent Relationship
The median ET across all centers and cycle types was 8.9 mm. However, notable regional differences were observed: the median was 9.0 mm in the USA, 8.7 mm in Spain, and 8.0 mm in the UAE. These variations underscore the potential for inter-center and inter-observer differences in ultrasound measurement.
The 7 mm Threshold in Programmed and Modified Natural Cycles
When the data from all centers were aggregated, the results revealed a clear decline in LBR when the ET was less than 7 mm in both programmed and modified natural cycles. Specifically, the regression analysis showed:
The Natural Cycle Exception
Intriguingly, the study found that for patients undergoing a pure natural cycle (NC), there was no identified ET threshold at which LBR was significantly impacted. In these cases, even an ET <7 mm did not correlate with a statistically significant reduction in LBR (aOR 0.85; 95% CI 0.58-1.25, P = 0.41). This finding suggests that the physiological hormonal milieu of a natural cycle may compensate for a thinner endometrial lining, or perhaps that thickness is a less reliable surrogate for receptivity in the absence of exogenous hormonal manipulation.
Predictive Limitations of ET
Despite the statistical significance of the <7 mm threshold in certain protocols, the study highlighted a critical clinical reality: ET is a poor predictor of individual success. The Area Under the Curve (AUC) for a model including ET (0.597) was not significantly better than a model without it (0.591). This indicates that while a thin endometrium may lower the statistical probability of success, it cannot reliably predict which individual patients will or will not achieve a live birth.
Expert Commentary: Clinical and Biological Implications
The results of this study suggest that the ‘ideal’ thickness is a moving target influenced by the preparation protocol. The decline in LBR in programmed and mNC cycles at the 7 mm mark provides a useful clinical benchmark, but the lack of impact in NC cycles is a point of significant biological interest.
Biological Plausibility
Why does ET matter less in a natural cycle? One hypothesis is that natural cycles involve a more synchronized development of the endometrial functionalis and vascularization, driven by endogenous follicle-stimulating hormone (FSH) and luteinizing hormone (LH). In contrast, programmed cycles rely on exogenous steroids which might lead to a dissociation between morphological thickness and functional receptivity. Furthermore, the higher doses of estrogen used in programmed cycles can sometimes lead to a ‘thick’ but poorly receptive environment, whereas a ‘thin’ natural lining might be perfectly functional.
Standardization Challenges
The regional variations in median ET (ranging from 8.0 mm to 9.0 mm) highlight the inherent subjectivity of ultrasound measurements. Clinicians must consider that a 6.5 mm measurement in one clinic might be equivalent to a 7.5 mm measurement in another due to equipment calibration, ultrasound probe angle, and technician experience. This variability suggests that clinical decisions—such as cycle cancellation—should not be based solely on a single millimeter difference.
Conclusions and Practical Recommendations
The study by Genovese et al. provides several key takeaways for the modern fertility specialist:
1. Protocol Selection Matters
In patients who persistently demonstrate a thin endometrium (<7 mm) in programmed cycles, switching to a natural cycle may be a viable strategy, as thickness appears to have less impact on LBR in this protocol.
2. Avoid Arbitrary Cancellations
Given the poor predictive value of ET for individual live birth (low AUC), clinicians should be cautious about canceling euploid transfers based solely on a lining measurement of 6 mm or 7 mm, especially if the embryo is of high quality and the patient has limited options.
3. Regional and Institutional Context
Clinics should be aware of their own median ET measurements and success rates to better counsel patients on what constitutes a ‘thin’ lining within their specific practice environment.
Summary of Evidence
While this retrospective study cannot establish causality, its sheer scale—over 30,000 euploid cycles—provides the most robust data to date on the relationship between ET and LBR. The findings reinforce the 7 mm threshold as a point of concern in programmed cycles but offer a more optimistic outlook for thin linings in natural cycles. Ultimately, endometrial thickness is but one piece of the complex puzzle of implantation, and its importance must be weighed alongside embryo quality, protocol type, and patient history.
References
Genovese H, Mayo CA, Kalafat E, Fatemi H, Ata B, Garcia-Velasco J, Seli E. Does endometrial thickness impact live birth rate following a frozen embryo transfer: outcomes of 30 676 euploid single embryo transfers. Hum Reprod. 2025 Oct 1;40(10):1919-1927. doi: 10.1093/humrep/deaf129. PMID: 40639807.