Introduction: The Quest for Superior Renal Protection
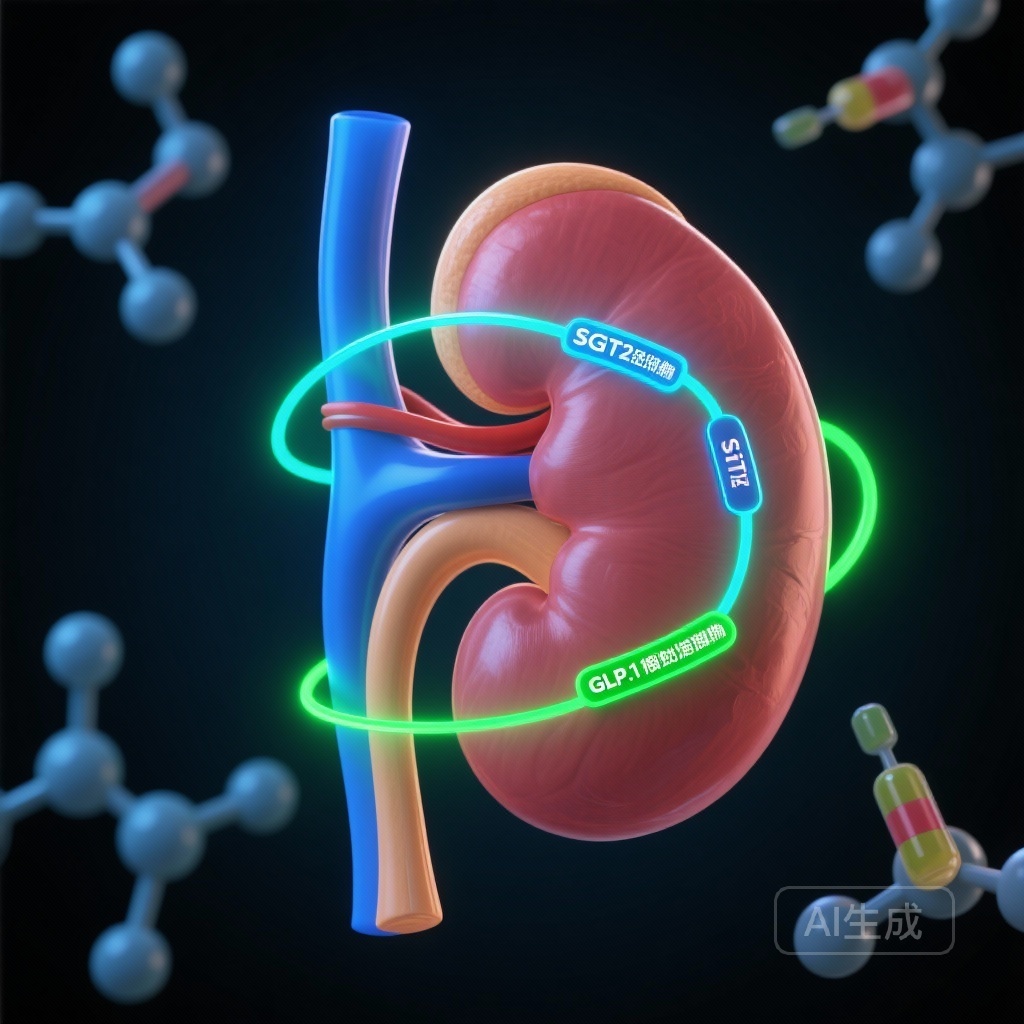
For decades, the management of type 2 diabetes (T2D) focused primarily on glycemic control. However, the paradigm has shifted toward organ protection, specifically targeting cardiovascular and renal outcomes. Sodium-glucose cotransporter-2 inhibitors (SGLT2i) and glucagon-like peptide-1 receptor agonists (GLP-1RA) have emerged as the twin pillars of modern metabolic therapy. While both classes have demonstrated significant renal benefits in placebo-controlled trials, clinicians have long faced a dilemma: which agent is more effective for preserving kidney function in a real-world setting? In the absence of direct head-to-head randomized clinical trials (RCTs), a new study published in JAMA Internal Medicine provides critical evidence using a target trial emulation design.
Highlights of the Comparative Effectiveness Study
The study, led by Jensen and colleagues, utilized nationwide Danish registry data to compare SGLT2i and GLP-1RA initiators. The primary findings indicate that SGLT2i treatment is associated with a significantly lower risk of chronic kidney disease (CKD) and acute kidney injury (AKI) compared to GLP-1RA treatment over a five-year follow-up period. Notably, the renal protective effects were most pronounced in individuals without pre-existing kidney disease, suggesting a powerful role for SGLT2i in the primary prevention of diabetic nephropathy.
The Clinical Burden of Diabetic Kidney Disease
Diabetic kidney disease (DKD) remains the leading cause of end-stage renal disease (ESRD) globally. Despite the standard use of renin-angiotensin system (RAS) inhibitors, many patients continue to experience a progressive decline in estimated glomerular filtration rate (eGFR). The introduction of SGLT2i and GLP-1RA offered new hope, yet their comparative efficacy remained a matter of debate. SGLT2i work primarily through hemodynamic mechanisms—reducing intraglomerular pressure—while GLP-1RAs are thought to exert nephroprotective effects through anti-inflammatory and metabolic pathways. Understanding which pathway offers better long-term outcomes is essential for personalizing T2D management.
Study Design and Methodology: Emulating the Gold Standard
To address the lack of head-to-head RCT data, the researchers employed a target trial emulation design. This methodology applies RCT-like rigor to observational data, minimizing common biases such as immortal time bias and selection bias. The study included 36,279 individuals initiating an SGLT2i and 18,782 initiating a GLP-1RA in Denmark between 2014 and 2020. All participants were previously treated with metformin, ensuring a relatively homogeneous baseline.
Endpoints and Statistical Rigor
The two coprimary outcomes were carefully defined. Chronic kidney disease (CKD) was defined as a composite of a 40% reduction in eGFR, severe albuminuria, or kidney failure. Acute kidney injury (AKI) was assessed using mean cumulative counts (MCCs) to account for the possibility of multiple events per individual. To ensure comparability between groups, the researchers used inverse probability of treatment weights (IPTW), adjusting for a wide array of baseline characteristics including age, sex, diabetes duration, comorbidities, and baseline renal function.
Key Findings: SGLT2i vs. GLP-1RA
The results provide a clear signal for renal outcomes. The weighted 5-year risk of CKD was 6.7% for those starting an SGLT2i compared to 8.2% for those starting a GLP-1RA. This translates to a risk ratio (RR) of 0.81 (95% CI, 0.76-0.87), representing a 19% relative risk reduction in favor of SGLT2i. The absolute risk difference was -1.5%, indicating that for every 67 patients treated with an SGLT2i instead of a GLP-1RA, one case of CKD could be prevented over five years.
The Impact on Acute Kidney Injury
One of the most striking findings was the reduction in AKI burden. The 5-year MCC of AKI per 100 individuals was 25.2 for SGLT2i and 28.7 for GLP-1RA. The MCC ratio of 0.88 (95% CI, 0.83-0.93) suggests that SGLT2i initiators experienced 12% fewer AKI events. This finding is particularly important given earlier concerns that SGLT2i might increase AKI risk due to their initial hemodynamic effect on the glomerulus; this study reinforces the growing consensus that SGLT2i are actually protective against AKI.
Secondary Outcomes: A Nuanced Picture
While SGLT2i led the way in CKD and AKI prevention, the secondary outcomes revealed a more complex interaction. GLP-1RA initiators showed slightly better outcomes regarding the reduction of albuminuria and overall mortality. This suggests that while SGLT2i may be superior for preserving GFR and preventing acute tubular damage, GLP-1RAs might offer distinct advantages in reducing protein excretion and providing broader cardiovascular or metabolic benefits that impact survival.
Subgroup Analysis: Primary vs. Secondary Prevention
The researchers conducted stratification based on pre-existing cardiovascular and kidney disease. The most pronounced reductions in CKD and AKI with SGLT2i were observed among individuals without pre-existing kidney disease at baseline. This highlights the potential of SGLT2i as a primary preventive strategy, intervening early in the disease course to prevent the onset of structural renal damage.
Expert Commentary and Mechanistic Insights
Why did SGLT2i outperform GLP-1RAs in these specific renal metrics? Experts point to the unique hemodynamic effects of SGLT2 inhibition. By inhibiting glucose and sodium reabsorption in the proximal tubule, these agents increase sodium delivery to the macula densa, which restores tubuloglomerular feedback and causes afferent arteriolar vasoconstriction. This reduces glomerular hyperfiltration—a hallmark of early diabetic nephropathy.
In contrast, GLP-1RAs likely work through different channels. They reduce systemic inflammation, oxidative stress, and blood pressure, which may explain their superior performance in reducing albuminuria—a marker of endothelial dysfunction—and mortality. The clinical implication is that these two classes may be complementary rather than mutually exclusive, though for a patient whose primary risk is a declining eGFR, SGLT2i may be the preferred starting point.
Study Limitations
Despite the robust design, the study has limitations inherent to observational data. Residual confounding remains a possibility, and the study was conducted in a predominantly white Danish population, which may limit generalizability to other ethnic groups. Furthermore, the definition of CKD relied on registry data, which may not capture every minor fluctuation in eGFR.
Conclusion: Shaping Future Guidelines
The Jensen et al. study provides the strongest evidence to date that SGLT2 inhibitors are superior to GLP-1 receptor agonists for preventing hard renal endpoints like CKD progression and AKI in a real-world T2D population. These findings support the early initiation of SGLT2i, especially for patients at high risk of renal decline. As clinical guidelines continue to evolve, this study underscores the importance of choosing the right tool for the specific clinical goal: SGLT2i for renal filtration preservation and GLP-1RAs for albuminuria control and cardiovascular risk reduction.
References
Jensen SK, Heide-Jørgensen U, Andersen IT, Bonnesen K, Fu EL, Thomsen RW, Christiansen CF. SGLT2 Inhibitors vs GLP-1 Receptor Agonists for Kidney Outcomes in Individuals With Type 2 Diabetes. JAMA Intern Med. 2026; doi:10.1001/jamainternmed.2025.7409.