Highlights
– Reticulated platelets (RPs) from 95 coronary artery disease (CAD) patients show elevated activation markers and enrichment of prothrombotic pathways compared with paired mature platelets.
– Multi-omic profiling identified upregulation of GP6 (GPVI), TBXA2R (thromboxane receptor), and VWF transcripts, novel GPVI splicing and RP-specific non-coding RNAs, including circRNAs.
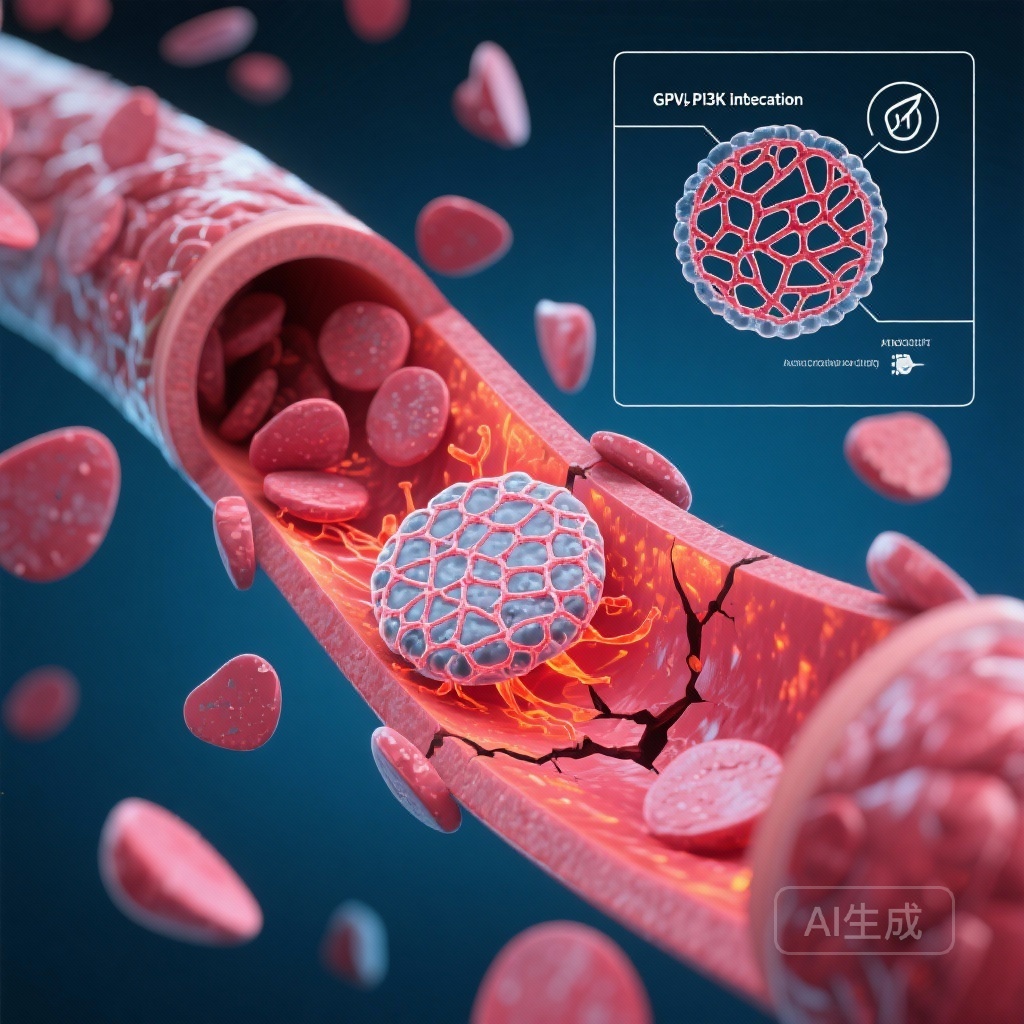
– Proteomic and functional assays show amplified PI3K–AKT and SYK phosphorylation, higher reactive oxygen species (ROS), greater aggregation, spreading and thrombus recruitment, which are attenuated by PI3K inhibitor LY294002 and GPVI antibody glenzocimab.
Background and clinical context
Despite progress in antiplatelet therapy, thrombotic complications remain a leading cause of morbidity and mortality in patients with coronary artery disease (CAD). Platelet heterogeneity — specifically the presence of reticulated platelets (RPs), newly produced, RNA-containing, hyperreactive platelets — has been implicated in heightened thrombotic risk and in reduced response to conventional antiplatelet agents. Automated hematology indices such as the immature platelet fraction (IPF) are increasingly reported in clinical samples, but mechanistic understanding and therapeutic implications of RP biology in human CAD are incompletely defined.
Study design and methods
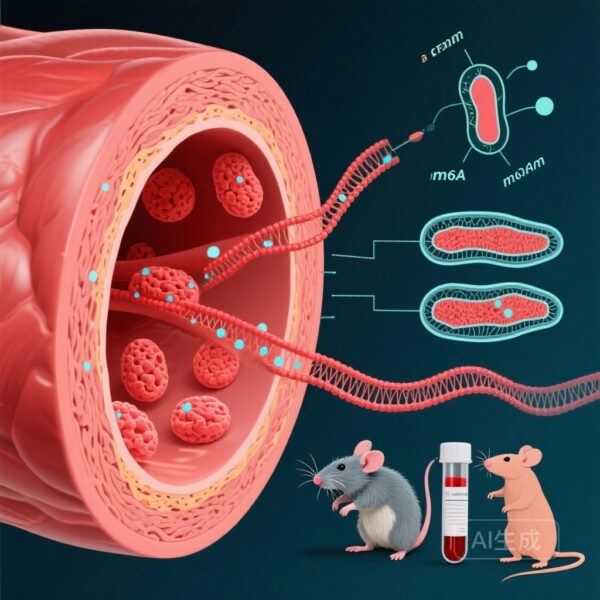
The publication by Kirmes et al. reports a comprehensive, multidimensional characterization of RPs in CAD. In 95 patients with documented CAD, reticulated platelets and paired mature platelets were isolated by RNA content and CD41 expression, enabling within-donor comparisons to control for interindividual variability. The investigators integrated bulk transcriptomics (RNA-seq) with high-dimensional proteomics using mass cytometry, followed by functional validation in independent cohorts.
Functional assays included flow cytometry–based platelet–platelet binding, in vitro thrombosis models under flow, platelet spreading assays, intracellular phospho-protein profiling, and reactive oxygen species (ROS) measurements. Pharmacologic perturbations used the PI3K inhibitor LY294002 (a research-grade tool compound) and glenzocimab, a monoclonal antibody targeting GPVI (a clinically advanced GPVI antagonist).
Results and datasets were curated into Platlas, an open-access web resource described by the authors to permit broader interrogation of RP-specific molecular features.
Key findings
Distinct transcriptomic signature of RPs
In paired analyses, RPs demonstrated a robust enrichment of transcripts related to platelet activation and thrombotic function. Notably, transcripts encoding GP6 (the gene for the platelet collagen receptor GPVI), TBXA2R (thromboxane A2 receptor) and VWF were elevated in RPs compared with mature platelets (MPs). The RNA-seq data also revealed previously unreported GPVI splice variants and a catalogue of RP-enriched non-coding RNAs, including novel circular RNAs (circRNAs). The presence of these RNA species supports an active and distinct transcriptomic program in the youngest circulating platelets.
Proteomic corroboration and signalling amplification
Mass cytometry and phospho-protein profiling aligned with transcriptomic findings: RPs showed higher surface expression of classical activation markers and augmented signalling through PI3K–AKT and SYK pathways. Increased phosphorylation of PI3K, AKT and SYK kinases was consistently observed in RPs. In addition, RPs produced higher levels of ROS, which can amplify platelet activation and thrombus propagation.
Enhanced functional thrombogenicity of RPs
Functionally, RPs exhibited greater aggregation responses, more rapid and extensive spreading on adhesive substrates, and disproportionately higher recruitment into growing thrombi under flow. In assays modelling thrombosis, RPs were more likely to adhere, aggregate and contribute to thrombus mass than paired mature platelets from the same donor.
Targeted inhibition reduces RP hyperreactivity
Importantly, pharmacologic inhibition of PI3K with LY294002 and blockade of GPVI with glenzocimab substantially attenuated RP-driven functional endpoints. Both interventions reduced platelet aggregation, spreading and recruitment into thrombi in ex vivo assays. These observations provide mechanistic evidence that GPVI and PI3K signalling nodes are key contributors to RP hyperreactivity and are potentially targetable to blunt RP-mediated thrombogenicity.
Validation and resources
The authors validated molecular and functional signatures in independent cohorts and made curated data available through Platlas, which the paper describes as an interactive, open-access resource to explore RP-specific transcripts, proteins and signaling networks. This facilitates external interrogation and hypothesis generation for translational studies.
Clinical and translational implications
The study provides a plausible mechanistic link between elevated reticulated platelets and adverse thrombotic outcomes in CAD: RPs are not merely markers of increased platelet turnover but are functionally distinct cells with amplified GPVI and PI3K-driven signalling. Several clinical implications follow.
First, measurement of RP burden or IPF could become a meaningful biomarker to identify patients at increased thrombotic risk or those with higher residual platelet reactivity on standard antiplatelet regimens (e.g., aspirin plus P2Y12 inhibitors). Second, the results nominate GPVI — an attractive antiplatelet target because it is platelet-restricted and important for collagen-mediated activation — and PI3K signalling as mechanistic intervention points. Glenzocimab (an anti-GPVI monoclonal antibody) is already in clinical development for arterial thrombosis and neurovascular indications; these data strengthen its rationale in RP-driven CAD. Third, PI3K inhibitors available as research compounds highlight a biologic dependency, although clinical translation would require agents with acceptable safety profiles and careful bleeding-risk assessment.
Strengths of the study
Key strengths include a within-donor paired design that minimizes confounding by interindividual variability; integration of RNA-seq and proteomic phospho-signalling data providing mechanistic depth; functional validation across multiple assays of platelet activation and thrombosis; and replication in independent cohorts. The open-data approach (Platlas) enhances transparency and enables independent validation and secondary analyses.
Limitations and caveats
Several important limitations should be recognized. The study is ex vivo and mechanistic; it does not provide clinical outcome data linking RP molecular signatures to incident ischemic events in a prospective manner. Pharmacologic inhibitors used include LY294002, a tool compound not suitable for clinical use; therefore, the translation of PI3K inhibition requires clinical-grade agents and safety data. Glenzocimab has a favorable mechanistic rationale, but efficacy and bleeding-risk profiles in CAD populations stratified by RP burden remain to be established in randomized trials. Finally, the measurement of RPs and the practical implementation of RP-stratified therapy in routine care will require standardization of assays (e.g., IPF) and prospective validation as biomarkers.
Expert commentary and guideline context
Current guideline-directed antiplatelet therapy for CAD is principally informed by ischemic and bleeding risk stratification and does not incorporate measurements of platelet age or turnover. The 2020/2021 ESC guidelines for non–ST-elevation acute coronary syndromes emphasize individualized antiplatelet strategies but do not yet recommend therapy guided by RP measurements. The present work by Kirmes et al. adds a mechanistic rationale for future trials that integrate platelet turnover biomarkers into therapeutic algorithms, offering the potential for precision antiplatelet therapy. Any change in practice will, however, require randomized evidence showing improved clinical outcomes without unacceptable bleeding.
Future directions
Priority next steps include: (1) prospective clinical studies correlating RP burden and the Platlas-derived molecular signatures with ischemic and bleeding outcomes in patients on standard antiplatelet regimens; (2) early-phase clinical trials of GPVI antagonists (for example glenzocimab) in CAD patients enriched for high RP burden to test efficacy and safety; (3) development or repurposing of clinically viable PI3K pathway modulators with favorable therapeutic windows; (4) standardization and regulatory qualification of RP/IPF as a biomarker; and (5) exploration of RP-specific non-coding RNAs (including circRNAs) as circulating biomarkers or therapeutic targets.
Conclusions
Kirmes et al. deliver a multidimensional mechanistic explanation for the hyperreactivity of reticulated platelets in CAD, demonstrating a distinct transcriptomic and proteomic profile characterized by upregulated GPVI and PI3K signalling and enhanced functional thrombogenicity. The attenuation of RP-driven thrombosis by GPVI and PI3K inhibition supports the concept of mechanism-guided antiplatelet strategies tailored to platelet turnover. Translation into clinical practice will require prospective outcome studies, assay standardization, and careful assessment of bleeding risk in intervention trials.
Funding and trial registration
Details on funding and any trial registrations are reported in the original publication (see reference below).
References
1. Kirmes K, Han J, Klug M, Bloxham CJ, Babyak O, Bernett J, Arend L, Manz Q, Raka L, Schwartz L, Hoffmann M, Rosenbaum M, Ruland J, Ciora OA, Louadi Z, Tsoy O, Newaz K, Modica J, Conca Dioguardi C, Peano C, Müller M, Santovito D, Viggiani G, Kühne S, von Scheidt M, Nicolai L, Wu T, Baumbach J, Chiarito M, Laugwitz KL, Condorelli G, Raake PWJ, List M, Bernlochner I, Bongiovanni D. Reticulated platelets in coronary artery disease: a multidimensional approach unveils prothrombotic signalling and novel therapeutic targets. Eur Heart J. 2025 Dec 1;46(45):4901-4917. doi: 10.1093/eurheartj/ehaf694. PMID: 40886063; PMCID: PMC12665372.
2. Collet JP, Thiele H, Barbato E, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST‑segment elevation. Eur Heart J. 2021;42(14):1289–1367. doi:10.1093/eurheartj/ehaa575.
Author note
This article synthesizes and interprets the findings from Kirmes et al. for a clinical and translational audience. It aims to place mechanistic discoveries about reticulated platelets into the context of potential clinical applications and the pathway toward precision antiplatelet strategies in coronary artery disease.