Introduction
In the management of early-onset severe hemolytic disease of the fetus and newborn (HDFN), the therapeutic landscape has long been limited to invasive procedures such as intrauterine transfusions (IUTs). However, the emergence of neonatal Fc receptor (FcRn) blockers, specifically nipocalimab, offers a novel pharmacological pathway to mitigate maternal-to-fetal transfer of pathogenic alloantibodies. A critical concern with this mechanism is the potential impact on the infant’s developing immune system, given that FcRn is essential for the placental transfer of protective maternal immunoglobulin G (IgG). The UNITY study provides pivotal data on the pharmacokinetic profile of nipocalimab and the subsequent immunological health of infants exposed in utero.
Highlights
Minimal Fetal Drug Exposure
Despite therapeutic maternal concentrations of nipocalimab, the drug was largely undetectable or found at extremely low levels in fetal cord blood and breast milk, suggesting limited direct fetal exposure.
Transient Hypogammaglobulinemia
Infants exhibited low IgG levels at birth (median 175 mg/dl), which reached a physiological nadir by 24 weeks but recovered to normal ranges between 16 and 96 weeks of age.
Preserved Vaccine Efficacy
Clinical data confirmed that infants developed protective antibody titers to standard vaccinations, such as diphtheria and tetanus, despite the initial period of low IgG.
Background: The Burden of Severe HDFN
Hemolytic disease of the fetus and newborn remains a significant cause of fetal morbidity and mortality. It occurs when maternal IgG alloantibodies—most commonly anti-D or anti-K—cross the placenta and target fetal red blood cell antigens, leading to severe anemia, hydrops fetalis, and potential fetal loss. Currently, the standard of care for early-onset cases (occurring before 24 weeks’ gestation) involves serial IUTs, which are technically demanding and carry risks of procedural complications.
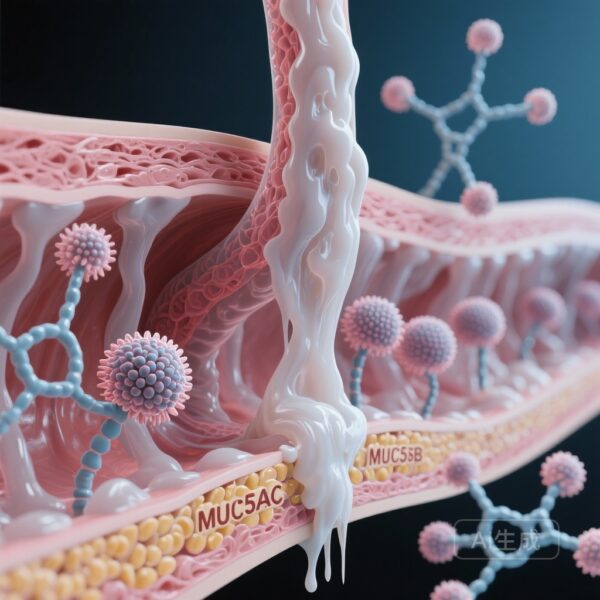
Nipocalimab is a high-affinity, fully human, aglycosylated IgG1 monoclonal antibody designed to block the FcRn. By occupying the FcRn binding site, nipocalimab achieves two goals: it accelerates the clearance of maternal pathogenic IgG and simultaneously blocks the placental transfer of these antibodies to the fetus. While this mechanism is therapeutically elegant, it raises a fundamental clinical question: does the systemic reduction of maternal IgG and the blockade of placental transfer leave the newborn vulnerable to infections or impair their long-term immune development?
Study Design and Methodology
The UNITY study was a single-group, open-label, phase 2 clinical trial that enrolled pregnant individuals at high risk for early-onset severe HDFN. Participants received weekly intravenous infusions of nipocalimab (30 or 45 mg/kg) starting as early as 14 weeks and continuing up to 35 weeks of gestation.
The primary objectives reported in this analysis focused on the safety and pharmacokinetics of the drug in the mother-infant dyad. Researchers measured nipocalimab concentrations in maternal blood, fetal cordocentesis samples, cord blood at delivery, and postpartum breast milk. Neonatal immune health was monitored through longitudinal assessments of serum IgG levels, the incidence of infectious adverse events, and the ability to mount an immune response to standard childhood vaccinations through 96 weeks of life.
Key Findings: Pharmacokinetics and Neonatal Immunity
Pharmacokinetic Profile
Maternal participants maintained pharmacologically active concentrations of nipocalimab (defined as >10 μg/ml) throughout the dosing interval. However, the transfer of the drug across the placenta appeared highly restricted. In fetal cordocentesis, only one of four samples showed detectable drug (0.04 μg/ml). Similarly, at birth, only one of eleven cord blood samples showed a trace amount (0.7 μg/ml). This suggests that while nipocalimab effectively blocks the transfer of other IgG molecules by occupying the FcRn, the drug itself does not cross the placental barrier in significant quantities.
Furthermore, analysis of colostrum and breast milk revealed very low concentrations of nipocalimab, with most samples falling below the limit of quantification. This indicates that breastfeeding is unlikely to result in significant systemic drug exposure for the infant.
Immunoglobulin G Recovery
As expected by the mechanism of action, infants born to mothers treated with nipocalimab had significantly lower IgG levels at birth compared to historical norms. The median cord blood IgG was 175 mg/dl, reflecting the successful blockade of maternal IgG transfer. This level further decreased to a physiologic nadir by 24 weeks (median 273 mg/dl).
Crucially, the study observed a robust recovery of IgG levels as the infants began their own endogenous production of antibodies. Between 16 and 96 weeks, the median IgG rose to 762 mg/dl, with nearly all infants reaching the normal range for their age. This confirms that the antenatal blockade of FcRn does not permanently impair the infant’s intrinsic ability to synthesize immunoglobulins.
Clinical Safety and Infectious Outcomes
Safety analysis included 12 live-born infants. The incidence of infections was a primary concern; however, the study found that most infectious adverse events were mild to moderate and consistent with typical childhood illnesses (e.g., upper respiratory tract infections). There were no reports of unusual, opportunistic, or life-threatening infections that would suggest a state of profound or prolonged immunodeficiency.
Vaccine Response
The ability of the infant immune system to respond to active immunization is a hallmark of functional immunity. In this cohort, six of seven infants assessed at or before 96 weeks demonstrated protective titers against diphtheria and tetanus. This finding is particularly reassuring for clinicians, as it suggests that the transient period of low maternal-derived IgG does not interfere with the infant’s capacity to respond to primary vaccination series.
Expert Commentary
The UNITY study results provide a reassuring safety signal for the use of FcRn blockers in pregnancy. The most significant finding is the disconnect between the low IgG levels at birth and the absence of severe clinical infectious sequelae. In neonatal medicine, we often rely on maternally derived IgG to provide passive immunity during the first few months of life. While nipocalimab disrupts this passive transfer, the data suggests that the infant’s immune system is resilient and capable of managing this transition without an increased risk of severe pathology.
However, it is important to note the small sample size (n=12). While these results are promising, larger phase 3 trials (such as the ongoing AZALEA study) will be necessary to confirm these findings across a more diverse population. Clinicians should also remain vigilant during the first six months of life, ensuring that these infants receive prompt evaluation for any signs of infection during their period of transient hypogammaglobulinemia.
From a mechanistic perspective, the low drug levels in cord blood are fascinating. It suggests that nipocalimab’s binding to FcRn in the syncytiotrophoblast may be so high-affinity that the drug remains sequestered or is degraded rather than being transcytosed into the fetal circulation. This “placental sink” effect could be a protective factor for the fetus.
Conclusion
Antenatal treatment with nipocalimab represents a potential paradigm shift in the management of severe HDFN, offering a non-invasive alternative to intrauterine transfusion. This follow-up study demonstrates that while the drug effectively blocks maternal IgG transfer—leading to low neonatal IgG at birth—the effect is transient. The lack of significant drug transfer to the fetus, the recovery of endogenous IgG production, and the successful response to vaccinations support the safety profile of nipocalimab regarding infant immunity. These findings provide a strong foundation for the continued development of FcRn-targeted therapies in high-risk pregnancies.
Funding and Clinical Trial Information
This study was funded by Johnson & Johnson. ClinicalTrials.gov number: NCT03842189.
References
1. de Winter DP, Moise KJ, et al. Infant Immunity after Maternal Nipocalimab in Severe Hemolytic Disease of the Fetus and Newborn. NEJM Evid. 2026 Feb;5(2):EVIDoa2500097.
2. Ling LE, et al. Nipocalimab for the Treatment of Early-Onset Severe Hemolytic Disease of the Fetus and Newborn. New England Journal of Medicine. 2024;390(22):2050-2060.
3. Moise KJ Jr. Hemolytic disease of the fetus and newborn: modern management. Part I. Genetic and clinical factors. American Journal of Obstetrics and Gynecology. 2008;198(4):352-361.