Executive Summary and Key Highlights
Long-term management of relapsing multiple sclerosis (RMS) has increasingly shifted toward the early utilization of high-efficacy disease-modifying therapies (DMTs). Among these, B-cell depletion via anti-CD20 monoclonal antibodies has become a cornerstone of treatment. The ULTIMATE I and II trials recently provided critical five-year data through their open-label extension (OLE), offering insights into the long-term efficacy and safety of ublituximab. The findings reinforce a proactive treatment paradigm, demonstrating that sustained ublituximab therapy leads to profound suppression of inflammatory activity and tangible benefits in disability outcomes.
Key highlights from the five-year analysis include:
1. Sustained Low Relapse Rates: Participants treated continuously with ublituximab (UBL-UBL) achieved an annualized relapse rate (ARR) of 0.020 by year 5, equivalent to just one relapse every 50 patient-years.
2. Rapid Improvement After Switching: Patients who switched from teriflunomide to ublituximab (TER-UBL) experienced a 58.4% reduction in ARR within the first year of the switch, with continued declines thereafter.
3. Disability Benefits: Continuous ublituximab therapy was associated with a significantly lower risk of 24-week confirmed disability progression (CDP24) and a higher likelihood of 24-week confirmed disability improvement (CDI24) compared to those who started on teriflunomide.
4. Stable Safety Profile: The incidence of serious infections remained low and stable over five years, with no new safety signals emerging despite long-term B-cell depletion.
The Evolving Landscape of Multiple Sclerosis Management
Multiple sclerosis (MS) is a chronic, immune-mediated disease of the central nervous system characterized by inflammation, demyelination, and axonal loss. For decades, the standard of care involved a ‘step-up’ approach, starting with moderately effective therapies and only escalating to high-efficacy treatments upon evidence of breakthrough disease. However, emerging evidence suggests that this delay can lead to irreversible neurological damage.
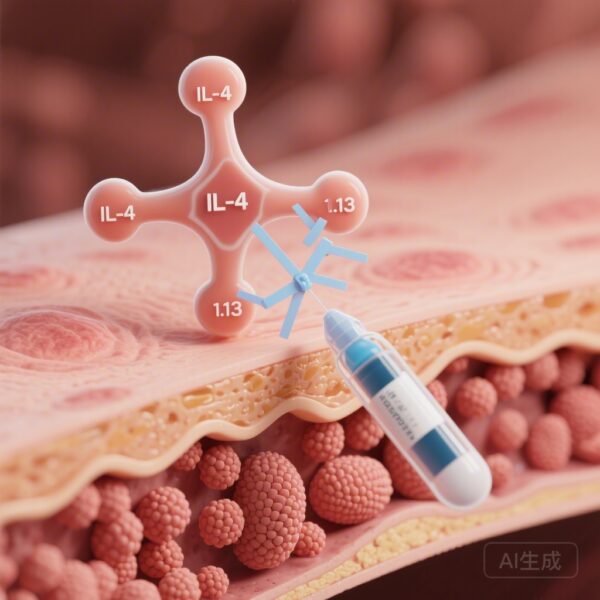
Ublituximab is a novel, glycoengineered anti-CD20 monoclonal antibody designed to target and deplete B-cells with high potency. By removing the fucose molecules from the antibody’s Fc region, ublituximab enhances its affinity for FcγRIIIa receptors on effector cells, such as natural killer cells. This results in potent antibody-dependent cellular cytotoxicity (ADCC), allowing for lower doses and shorter infusion times compared to earlier anti-CD20 therapies. The ULTIMATE I and II studies were designed to evaluate whether these mechanistic advantages translate into superior clinical outcomes over the long term.
Study Architecture: From Pivotal Trials to Long-Term Extension
The ULTIMATE I and II were identical Phase 3, multicenter, randomized, double-blind, active-controlled studies. They initially compared the efficacy and safety of ublituximab (450 mg every 24 weeks) against teriflunomide (14 mg daily) over a 96-week double-blind period (DBP). Following the completion of the DBP, eligible participants were invited to enter an ongoing open-label extension (OLE) study.
In the OLE, participants who were originally in the ublituximab group continued their treatment (the UBL-UBL cohort), while those in the teriflunomide group switched to ublituximab (the TER-UBL cohort). The primary objective of this extension was to evaluate the long-term safety and durability of the clinical response. The data cutoff for the current analysis was January 1, 2024, representing up to five years of cumulative follow-up for the original ublituximab group.
Clinical Efficacy: Sustained Suppression of Disease Activity
The five-year data reveal a striking and sustained reduction in disease activity. For the UBL-UBL cohort, the ARR, which was already low at the end of the DBP, continued to decrease. By year 3, the ARR was 0.053; by year 4, it was 0.032; and by year 5, it reached a remarkable 0.020. This trend suggests that prolonged B-cell depletion may provide cumulative benefits in stabilizing the disease.
For the TER-UBL cohort, the ‘switch’ data provided a powerful demonstration of ublituximab’s efficacy. Prior to the switch, these patients had an ARR of 0.182 on teriflunomide. Within the first year of switching to ublituximab, the ARR dropped to 0.076—a 58.4% reduction (P < .001). This suppression continued through the subsequent years, reaching 0.045 by year 5. While the TER-UBL group saw massive improvements, they did not quite reach the ultra-low ARR levels of the continuous UBL-UBL group, highlighting the 'head start' advantage of early high-efficacy therapy.
Impact on Disability: Progression and Improvement
Beyond relapses, the ULTIMATE OLE data focused on disability measures, which are often more meaningful to patients’ long-term quality of life. The study utilized two key metrics: Confirmed Disability Progression (CDP) and Confirmed Disability Improvement (CDI), both measured at 24-week intervals.
By year 5, the UBL-UBL group demonstrated a clear advantage in preventing disability worsening. The rate of CDP24 was 8.0% in the continuous ublituximab group compared to 14.3% in the TER-UBL group (P = .01). This suggests that the two-year delay in receiving high-efficacy therapy in the teriflunomide group resulted in a higher cumulative burden of disability that was not fully ‘caught up’ even after switching to ublituximab.
Furthermore, ublituximab appeared to facilitate neurological recovery in some patients. The CDI24 rate—representing a sustained improvement in Expanded Disability Status Scale (EDSS) scores—was 17.0% for the UBL-UBL cohort versus 12.2% for the TER-UBL cohort (P = .02). These data contribute to the growing body of evidence that high-efficacy DMTs may not only prevent damage but also provide a window for the nervous system to improve function by reducing the inflammatory ‘noise.’
Safety and Tolerability: A Five-Year Perspective
Safety is a paramount concern for long-term B-cell depletion, particularly regarding the risk of infections and changes in immunoglobulin levels. The five-year OLE data remained consistent with the safety profile established in the 2-year pivotal trials.
The exposure-adjusted incidence rates (EAIR) of serious infections (excluding COVID-19 events) were 2.10 per 100 participant-years for the UBL-UBL group and 2.58 for the TER-UBL group. Importantly, the study monitored serum immunoglobulin G (IgG) and IgM levels. While some decline in mean immunoglobulin levels is expected with anti-CD20 therapy, the levels in this study remained, on average, above the lower limit of normal (LLN). Furthermore, the researchers found no significant correlation between low immunoglobulin levels and the rate of serious infections during the study period.
Adverse events were generally manageable, with infusion-related reactions being the most common, primarily occurring during the first infusion. The long-term tolerability suggests that ublituximab is a viable option for chronic management in the RMS population.
Expert Commentary: The Clinical Case for Early High-Efficacy Therapy
The ULTIMATE OLE results add significant weight to the argument for ‘flipping the pyramid’ in MS treatment. Traditionally, clinicians waited for treatment failure before escalating to drugs like ublituximab. However, the disparity in CDP24 between the UBL-UBL and TER-UBL groups—despite both groups eventually being on the same potent medication—indicates that there is a critical therapeutic window early in the disease course.
From a mechanistic standpoint, the glycoengineering of ublituximab allows for efficient B-cell depletion even at lower protein doses, which may contribute to its favorable infusion profile. Clinically, the ARR of 0.020 is among the lowest reported in long-term extension studies of anti-CD20 therapies, suggesting that ublituximab is highly effective at maintaining a ‘no evidence of disease activity’ (NEDA) state.
However, clinicians must remain vigilant regarding long-term immune surveillance. While the five-year data are reassuring, the MS community continues to monitor for rare opportunistic infections and the impact of long-term B-cell depletion on vaccine efficacy. The stability of immunoglobulin levels in this cohort is a positive sign, but individualized monitoring remains the gold standard of care.
Conclusion: Reaffirming the Role of Ublituximab
The five-year results of the ULTIMATE I and II OLE reinforce ublituximab as a robust and effective long-term treatment option for patients with relapsing forms of multiple sclerosis. By maintaining exceptionally low relapse rates and significantly reducing the risk of disability progression, ublituximab meets the primary goals of modern MS therapy. The data specifically underscore the importance of early initiation, as patients who started on ublituximab from the beginning of the trial fared better than those who switched later. As the MS treatment landscape continues to evolve, these long-term data provide clinicians and patients with the confidence needed to make informed decisions about high-efficacy intervention.
Funding and Trial Registration
The ULTIMATE I and II studies and the subsequent Open-Label Extension were sponsored by TG Therapeutics, Inc.
Trial Registration: ClinicalTrials.gov Identifier: NCT04130997.
References
1. Cree BAC, Fox E, Hartung HP, et al. Five Years of Ublituximab in Multiple Sclerosis: ULTIMATE I and II Open-Label Extension Study. JAMA Neurol. 2026 Feb 16:e260007. doi: 10.1001/jamaneurol.2026.0007.
2. Hauser SL, Musch B, Meyer-Gersepach C, et al. Long-term safety and efficacy of ocrelizumab in relapsing multiple sclerosis: 10-year results from the OPERA open-label extension. Presented at ECTRIMS 2023.
3. Steinman L, Fox E, Hartung HP, et al. Ublituximab versus Teriflunomide in Relapsing Multiple Sclerosis. N Engl J Med. 2022;387(8):704-714. doi:10.1056/NEJMoa2201983.