Highlight
Reduced Acute Morbidity
IMPT was associated with a significantly lower incidence of grade 2 or higher acute toxicities compared to IMRT (86.6% vs 97.8%, p = 0.009).
Oncologic Equivalence
There were no statistically significant differences in 5-year cumulative incidence of local or regional failures, progression-free survival (PFS), or overall survival (OS) between the two modalities.
Late Toxicity Profile
While IMPT showed a numerically lower rate of grade 2+ late toxicities (40.3% vs 52.7%), the difference did not reach statistical significance in this cohort.
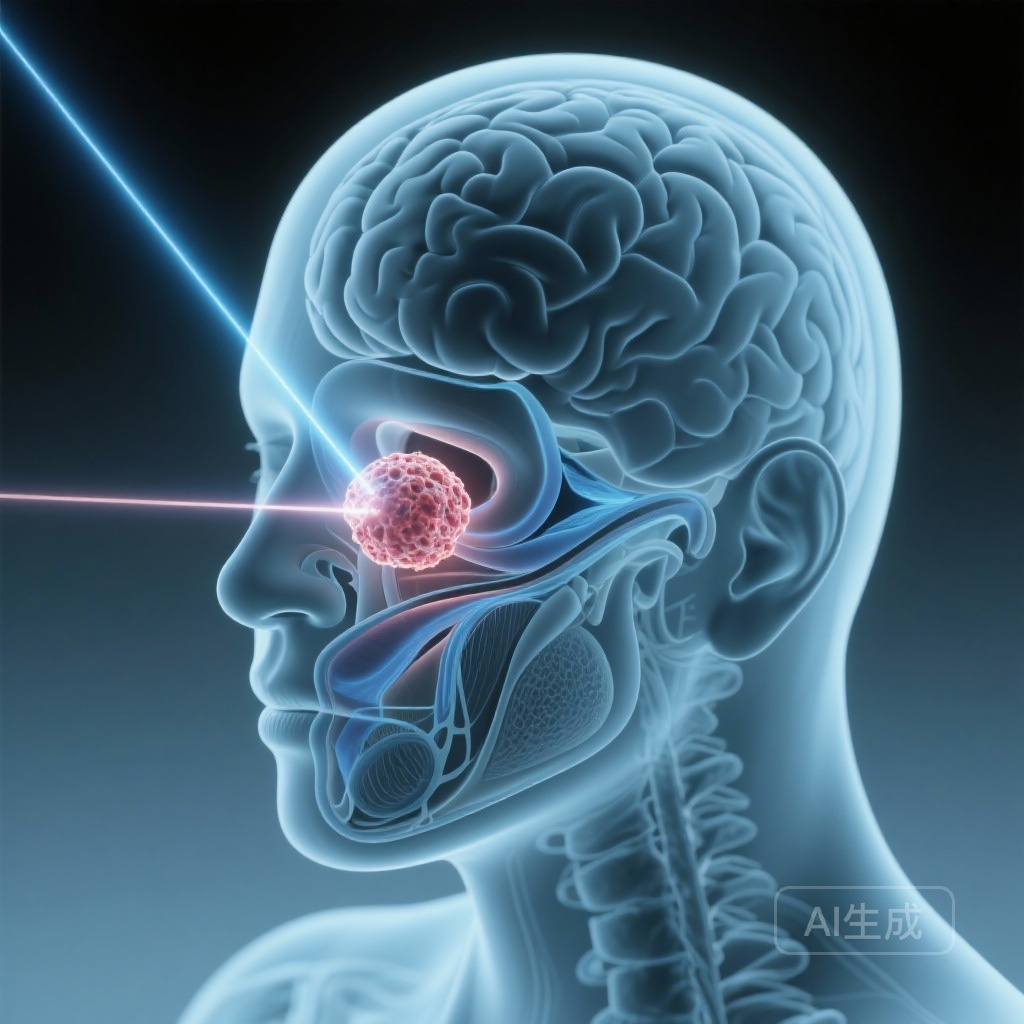
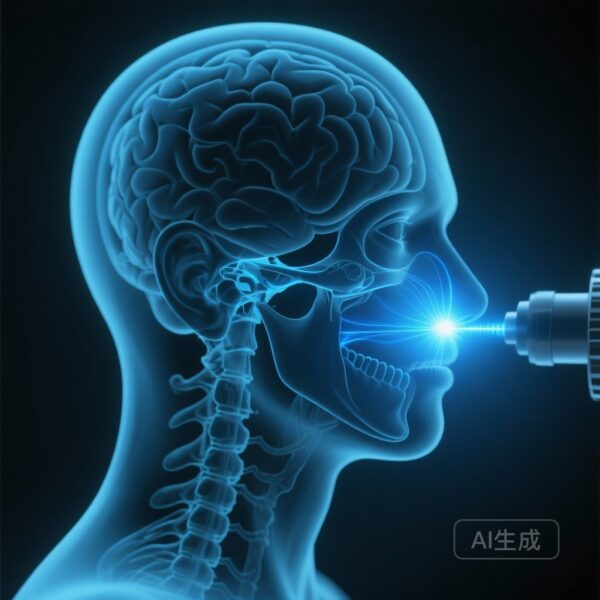
Background and Disease Burden
Nasopharyngeal carcinoma (NPC) presents a unique challenge in radiation oncology due to its complex anatomical location. Situated at the skull base, the nasopharynx is surrounded by critical OARs (organs at risk), including the brainstem, optic apparatus, salivary glands, and the oral cavity. While intensity-modulated radiotherapy (IMRT) has historically been the gold standard, providing excellent locoregional control, the exit dose of photon-based radiation often leads to significant acute and late toxicities.
Acute toxicities such as severe mucositis, xerostomia, and malnutrition can necessitate treatment interruptions, compromising oncological outcomes and patient quality of life. Intensity-modulated proton therapy (IMPT) offers a theoretical advantage through the physical properties of protons—specifically the Bragg peak. This allows for the delivery of high-dose radiation to the tumor while virtually eliminating the exit dose, potentially sparing healthy tissues located distal to the target. However, long-term comparative data between IMPT and IMRT have been limited, necessitating robust case-control analyses to validate these theoretical benefits in clinical practice.
Study Design and Methodology
This study, conducted at a tertiary academic cancer center between 2016 and 2022, employed a retrospective case-control design to evaluate the long-term efficacy and safety of IMPT versus IMRT in patients with nonmetastatic NPC. The cohort included 159 patients, with 67 (42.1%) receiving IMPT and 92 (57.9%) receiving IMRT.
The researchers focused on both acute toxicities (occurring during or shortly after treatment) and late toxicities (occurring months or years post-treatment). The primary endpoints included the incidence of grade 2 or higher toxicities according to the Common Terminology Criteria for Adverse Events (CTCAE). Secondary endpoints were oncological, including the 5-year cumulative incidence of local/regional failures, progression-free survival, and overall survival. The median follow-up time was 55.4 months, providing a substantial window to observe late-term effects and disease recurrence.
Key Findings: Safety and Acute Toxicity
The most striking result of the study was the significant reduction in acute morbidity in the IMPT group. The incidence of any grade 2+ acute toxicity was 86.6% for IMPT compared to 97.8% for IMRT (p = 0.009). This difference is clinically meaningful, as grade 2 toxicities often involve symptoms that interfere with daily activities or require medical intervention.
To further isolate the impact of the radiation modality, a logistic regression analysis was performed. The results indicated that the choice of radiotherapy modality (IMRT vs. IMPT) was a significant independent predictor of developing grade 2+ acute toxicity. Specifically, the odds ratio (OR) for IMPT was 0.177 (95% CI: 0.035-0.886; p = 0.035), suggesting a more than 80% reduction in the odds of experiencing significant acute side effects when using proton therapy.
Long-Term Oncologic Outcomes
Critics of new radiation technologies often express concern that sparing healthy tissue might inadvertently lead to marginal misses or reduced tumor control. However, this study reinforces the oncologic safety of IMPT. At the 5-year mark, the cumulative incidence of local or regional failures was nearly identical between the two groups: 14.1% for IMPT and 16.4% for IMRT (p > 0.05).
Furthermore, the study found no significant differences in progression-free survival or overall survival. These findings suggest that the precision of IMPT does not compromise the curative intent of the treatment. For clinicians, this provides reassurance that the reduction in acute toxicity does not come at the cost of long-term disease control.
Late Toxicity and Patient Quality of Life
Regarding late toxicities—those that often define the long-term survivorship experience—the IMPT group showed a lower percentage of grade 2+ complications (40.3%) compared to the IMRT group (52.7%). Although this 12.4% absolute reduction is clinically suggestive, it did not reach statistical significance in this specific study population (p > 0.05).
Common late toxicities in NPC treatment include chronic xerostomia, hearing loss, and neck fibrosis. The lack of statistical significance in late toxicity may be attributed to the sample size or the high baseline quality of modern IMRT plans, which already do a commendable job of sparing late-reacting tissues compared to older techniques. Nonetheless, the trend remains in favor of IMPT, and longer follow-up with larger cohorts may further clarify these benefits.
Expert Commentary
From a clinical perspective, the reduction in acute toxicity is the most compelling argument for IMPT in the treatment of NPC. Lower acute toxicity levels often translate to better patient adherence, fewer emergency department visits for dehydration or pain management, and a lower requirement for feeding tube placements.
The biological plausibility of these findings is rooted in the “low-dose bath” associated with IMRT. In photon therapy, the energy enters and exits the body, inevitably depositing low doses of radiation in the oral cavity and salivary glands. In contrast, IMPT stops at a predetermined depth, significantly reducing the integral dose to these sensitive structures.
However, it is important to acknowledge the limitations of this study. As a case-control study from a single tertiary center, there may be inherent selection biases. Additionally, the cost-effectiveness of IMPT remains a subject of intense debate. While the clinical benefits in the acute phase are clear, the higher capital and operational costs of proton facilities require that we continue to identify which specific patient subgroups derive the most benefit from this technology.
Summary and Conclusion
In conclusion, this case-control study provides robust evidence that IMPT is a safe and effective alternative to IMRT for patients with nonmetastatic nasopharyngeal carcinoma. The primary advantage of IMPT lies in its ability to significantly decrease the burden of acute grade 2+ toxicities, likely due to superior OAR sparing. Crucially, this reduction in side effects does not compromise 5-year oncological outcomes, including local control and overall survival.
While late toxicity differences were not statistically significant, the overall profile of IMPT suggests it is a valuable tool in the armamentarium of modern radiation oncology, particularly for improving the patient experience during the intensive course of NPC treatment. Future research should focus on prospective randomized trials and cost-utility analyses to further integrate IMPT into standard clinical pathways.
Funding and Acknowledgments
This research was supported in part by the National Institutes of Health/National Cancer Institute Cancer Center Support Grant P30 CA008748. The authors declare no conflicts of interest related to the funding of this study.
References
1. Intensity-modulated proton therapy vs intensity-modulated radiotherapy in nasopharyngeal carcinoma: a case-control study. (Study data provided).
2. Langendijk JA, et al. Selection of patients for particle therapy on the basis of expected reduction in toxicity-related health care costs. J Clin Oncol. 2013.
3. Lewis GD, et al. Cost-effectiveness Analysis of Intensity Modulated Proton Therapy Versus Intensity Modulated Photon Therapy for Maxillary Sinus Cancer. Int J Radiat Oncol Biol Phys. 2016.
4. Chua MLK, et al. Nasopharyngeal carcinoma. Lancet. 2016.