Introduction: The Endometrial Compaction Hypothesis
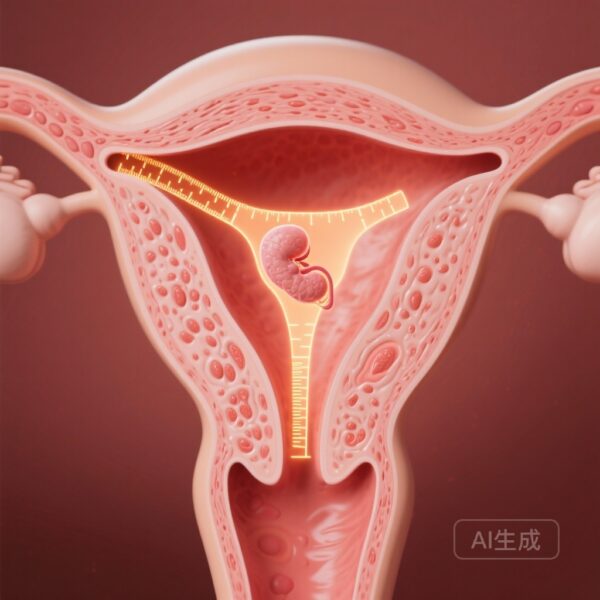
In the field of assisted reproductive technology (ART), the search for reliable non-invasive biomarkers of endometrial receptivity remains a priority. One of the most debated metrics in recent years is endometrial compaction—the phenomenon where the endometrial thickness (EMT) decreases following the administration of progesterone during a hormonal replacement therapy frozen-thawed embryo transfer (HRT-FET) cycle. Historically, some clinicians have viewed this thinning as a sign of successful progesterone-induced transformation from a proliferative to a secretory state, potentially signaling an optimal window of implantation. However, evidence has remained conflicting. A landmark retrospective analysis of over 16,000 cases, published in Human Reproduction Open, now provides substantial evidence that endometrial compaction is not associated with improved pregnancy outcomes and may, in specific contexts, be a negative prognostic indicator.
Highlights
1. Endometrial compaction (thinning) after progesterone administration is not associated with higher live birth rates in HRT-FET cycles.
2. In Day 3 embryo transfers, endometrial expansion—rather than compaction—is significantly associated with improved clinical pregnancy and live birth rates.
3. For blastocyst transfers, compaction may actually reduce the odds of achieving an HCG-positive result, suggesting that the developmental stage of the embryo interacts with endometrial dynamics.
4. The study suggests that current clinical preoccupations with achieving a ‘compacted’ endometrium may be unfounded, necessitating a shift toward stage-specific preparation protocols.
Background: The Role of Progesterone and EMT
The success of an embryo transfer depends on the synchronized dialogue between a high-quality embryo and a receptive endometrium. In HRT-FET cycles, exogenous estrogen is used to suppress dominant follicle development and thicken the endometrial lining. Once an adequate thickness is achieved, progesterone is introduced to trigger the secretory transformation required for implantation. It has been hypothesized that this transition causes the endometrial stroma to become denser, leading to a measurable decrease in thickness on ultrasound—a process termed ‘compaction.’ While some pilot studies suggested that compaction was a prerequisite for success, larger datasets have recently begun to question whether this morphological change is truly a surrogate for molecular receptivity.
Study Design and Methodology
This study represents a massive, single-center retrospective cohort analysis conducted at a high-volume fertility center between January 2018 and December 2022. The researchers analyzed a total of 16,453 FET cycles, subdivided into 9,390 Day 3 (D3) transfers and 7,063 blastocyst-stage transfers. To measure EMT changes, transvaginal ultrasounds were performed on two specific days: the day progesterone administration began (EMT1) and the day of the embryo transfer (ET) (EMT2).
Participants were categorized into three groups based on the change in EMT: the compaction group (where EMT decreased), the non-change group (where EMT remained stable), and the expansion group (where EMT increased). To ensure the findings were robust and to minimize the influence of confounding variables—such as maternal age, BMI, and embryo quality—the researchers utilized Inverse Probability Weighting (IPW) and stratified logistic regressions. This statistical rigor allows for a more accurate interpretation of the relationship between EMT dynamics and outcomes including HCG-positive rates, clinical pregnancy rates, live birth rates (LBR), and pregnancy loss.
Key Findings: Debunking the Compaction Advantage
The results of the analysis provide a clear departure from the ‘compaction is better’ narrative. Across both D3 and blastocyst transfers, the compaction group failed to show superior outcomes compared to those whose endometrium stayed the same or expanded.
Outcomes in Day 3 Embryo Transfers
In the D3 FET cohort, the data revealed a surprising trend: women in the compaction group actually had the lowest HCG-positive rates, clinical pregnancy rates, and live birth rates among the three groups. Specifically, the expansion group showed a positive association with improved LBRs (OR 1.166, 95% CI: 1.070-1.271). Furthermore, among patients who achieved a positive HCG, those in the compaction group experienced a higher rate of ectopic pregnancies (3.5% compared to 1.6% in the expansion group). This suggests that a thinning endometrium might not only be less receptive but could also influence the intrauterine environment in a way that affects embryo migration.
Outcomes in Blastocyst Transfers
For blastocyst-stage transfers, the impact of compaction was similarly underwhelming. Women in the compaction group had the lowest HCG-positive and clinical pregnancy rates. After IPW adjustment, the compaction group was associated with significantly lower odds of a positive HCG (OR 0.813) compared to the non-change group. Unlike the D3 cohort, however, the expansion group did not show a significantly higher LBR compared to the non-change group, though it still outperformed the compaction group in several metrics. The researchers noted that LBRs generally increased as the EMT change ratio rose, but only up to a certain threshold (30% for D3 and 50% for blastocysts), after which the benefit leveled off.
Expert Commentary: Biological Plausibility and Clinical Implications
The findings of Pan et al. (2025) suggest that the physiological response to progesterone is more complex than a simple thinning of the tissue. While progesterone does induce stromal decidualization, it also promotes vascularization and glandular secretion. In some patients, the expansion of the endometrium post-progesterone might reflect a robust secretory response or continued stromal proliferation that provides a more supportive environment for early-stage (D3) embryos. Conversely, significant compaction might indicate an over-accelerated maturation or a ‘hyper-progestin’ state that could potentially close the implantation window prematurely, particularly for blastocysts which require precise synchrony.
From a clinical perspective, these results are reassuring for both providers and patients. If a patient’s endometrium does not ‘compact’ after starting progesterone, there is no evidence to suggest the cycle should be canceled or that the prognosis is diminished. In fact, for D3 transfers, a slight expansion might be a favorable sign. This study underscores the need for ’embryo developmental stage-specific’ protocols. The uterine environment required for a cleavage-stage embryo, which must reside in the uterus for several days before implantation, may differ slightly from the environment required for a blastocyst ready to implant immediately.
Limitations and Future Directions
While the sample size of over 16,000 cases is a major strength, the study’s retrospective nature is a limitation. The embryos were not genetically tested (PGT-A), meaning embryo aneuploidy could remain a hidden variable, although the large sample size and IPW adjustment help mitigate this. Future prospective trials focusing on the molecular profile of the ‘expanding’ versus ‘compacting’ endometrium (using tools like RNA sequencing or the Endometrial Receptivity Array) would be valuable to correlate these ultrasound findings with actual transcriptomic markers of receptivity.
Conclusion
In conclusion, endometrial compaction is not a requisite for success in HRT-FET cycles. The expansion of the endometrium following progesterone administration is associated with improved live birth rates in Day 3 transfers, while compaction may be linked to lower success rates and higher ectopic risks. Clinicians should interpret EMT changes with caution and avoid using compaction as a primary determinant of cycle viability. These findings pave the way for more personalized and stage-specific endometrial preparation strategies in assisted reproduction.
Funding and References
This study was supported by the National Natural Science Foundation of China (82201856), the Basic Scientific Research project of Wenzhou Science and Technology Bureau (Y20220006), the Wenzhou Key Laboratory of Reproduction and Genetics (2022HZSY0051), and the Clinical Technology International Exchange Project of Zhejiang Provincial Medical Institutions.
Reference: Pan P, Liu C, Lin S, Wang H, Chen X, Yang H, Huang X, Zhang H, Teng Y. Endometrial compaction shows no association with improved pregnancy outcomes in hormonal replacement frozen-thawed embryo transfer: an analysis of over 16 000 cases. Hum Reprod Open. 2025 Jun 20;2025(3):hoaf039. doi: 10.1093/hropen/hoaf039.