Introduction
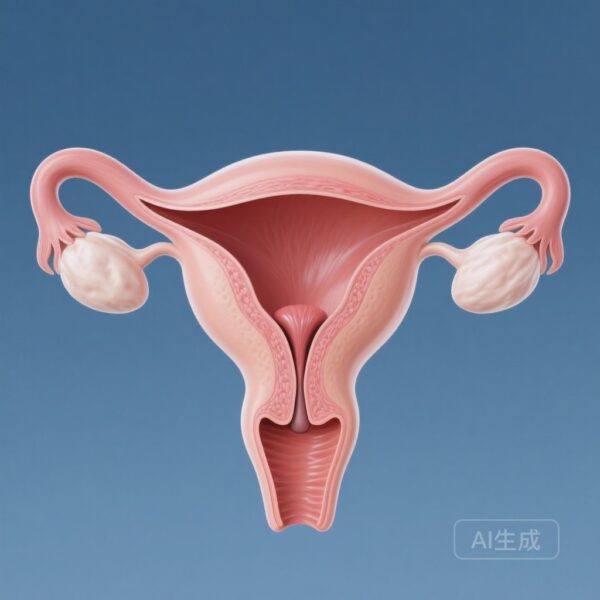
Low-grade endometrial stromal sarcoma (LG-ESS) represents a unique challenge in gynecologic oncology. While it is the second most common malignant uterine mesenchymal tumor, it is frequently characterized by a clinical course that is significantly more indolent than the aggressive leiomyosarcoma. However, this perceived indolence can be deceptive. A notable subset of patients faces significant morbidity, late recurrences, and even mortality, yet clinicians have long struggled to identify which tumors will behave aggressively. Two landmark studies published in 2025 provide critical insights into the clinicopathologic features that drive prognosis and the efficacy of traditional adjuvant treatments.
Highlights
- Cervical stromal involvement has been identified as a significant independent predictor of shorter recurrence-free survival (RFS) in LG-ESS patients.
- The presence of myxoid stroma and the lack of conventional morphology are associated with poorer oncologic outcomes.
- Large-scale SEER data analysis confirms that adjuvant external beam radiotherapy (EBRT) does not improve overall survival (OS) or cancer-specific survival (CSS) in LG-ESS.
- Surgical extensions such as lymphadenectomy and bilateral salpingectomy and oophorectomy (BSO) showed no significant survival benefit in retrospective cohorts, supporting a shift toward more conservative, individualized care.
The Clinicopathologic Spectrum: Insights from a 102-Tumor Cohort
Study Design and Population
In a comprehensive study by Devins et al. (2025), researchers evaluated 102 patients with LG-ESS, ranging in age from 21 to 74 years (median: 47). This study is particularly significant due to its depth of pathologic evaluation and long-term follow-up (median 79 months). All patients underwent hysterectomy and were staged using both the FIGO 2018 and 1988 systems.
Morphological Diversity and Growth Patterns
While 95% of the tumors exhibited conventional morphology resembling proliferative endometrial stroma, the study highlighted the striking heterogeneity of LG-ESS. Variants observed included:
- Fibroblastic appearance (n=35)
- Smooth muscle differentiation (n=23)
- Sex cord-like differentiation (n=21)
- Stromal hyalinization (n=21)
- Myxoid stroma (n=9)
Less common features such as glandular differentiation, deciduoid appearance, and even rhabdomyoblastic differentiation were noted, emphasizing that LG-ESS can mimic various other uterine pathologies, potentially leading to diagnostic pitfalls.
Predicting Recurrence and Survival
The 5-year recurrence-free survival (RFS) was 80%, but this dropped to 51% at 10 years, underscoring the necessity for long-term surveillance. Statistical analysis revealed that cervical stromal involvement (P=0.018) and myxoid stroma (P<0.001) were linked to shorter RFS. Interestingly, tumors lacking a conventional component altogether had worse disease-specific survival (DSS) (P=0.048). On multivariate analysis, cervical stromal involvement remained the only independent predictor of recurrence (HR: 16.939).
Evaluating Adjuvant Interventions: The SEER Analysis
Methods and Propensity Score Matching
Parallel to the pathologic findings, Jian et al. (2025) conducted a large-scale retrospective study using the Surveillance, Epidemiology, and End Results (SEER) database, analyzing 1,254 patients diagnosed between 2000 and 2021. To account for selection bias, the researchers utilized propensity score matching (PSM) to compare patients who received external beam radiotherapy (EBRT) with those who did not.
Survival Outcomes and Radiotherapy
The results were definitive: EBRT provided no survival benefit. Post-PSM, the Hazard Ratio (HR) for overall survival was 1.21 (95% CI 0.61-2.39), and for cancer-specific survival, it was 1.75 (95% CI 0.69-4.43). Neither radiotherapy, lymphadenectomy, nor BSO were associated with improved outcomes. Instead, prognosis was primarily driven by non-modifiable factors such as older age, larger tumor size, and advanced FIGO stage. Notably, the use of chemotherapy was associated with poorer outcomes, likely reflecting its use in the most aggressive or advanced cases rather than a lack of efficacy per se.
Expert Commentary: Shifting the Treatment Paradigm
The Challenge of Indolence
The findings from these two studies suggest that the traditional “one-size-fits-all” approach to LG-ESS management—often involving aggressive surgery and adjuvant radiation—may be unnecessary for many patients. The fact that tumors with only “minimal infiltration” can still recur decades later suggests that LG-ESS is a systemic or long-term biological process rather than a localized surgical problem.
Mechanistic Insights
The association of myxoid stroma and cervical involvement with poor outcomes may point to specific biological pathways or anatomical routes of spread that are not addressed by local radiotherapy. The lack of benefit from BSO in the SEER study is particularly provocative, as LG-ESS is traditionally considered highly hormone-sensitive. This suggests that while hormonal deprivation is a cornerstone of therapy, its impact on long-term survival in the context of modern surgical management requires further prospective validation.
Conclusion
LG-ESS remains a complex malignancy defined by its slow but persistent progression. The identification of cervical stromal involvement as a major independent risk factor provides clinicians with a new tool for risk stratification. Furthermore, the lack of evidence supporting the routine use of EBRT, lymphadenectomy, and BSO highlights an urgent need to move toward risk-adapted strategies that prioritize quality of life and avoid over-treatment. Future research should focus on molecular profiling to better understand the drivers of late recurrence and the potential for targeted therapies in patients with high-risk features like myxoid morphology or cervical involvement.
References
1. Devins KM, Mendoza RP, Shahi M, et al. Low-Grade Endometrial Stromal Sarcoma: Clinicopathologic and Prognostic Features in a Cohort of 102 Tumors. Am J Surg Pathol. 2025;49(10):977-991. doi:10.1097/PAS.0000000000002428.
2. Jian H, Guo J, Zhao W, et al. Prognostic Role of Radiotherapy in Low-Grade Endometrial Stromal Sarcoma: A SEER-Based Study. Cancer Control. 2025;32:10732748251356935. doi:10.1177/10732748251356935.