Highlights
- Vixarelimab demonstrated a significant, dose-dependent reduction in the Worst Itch Numeric Rating Scale (WI-NRS) at week 16, with the high-dose group achieving a 56.2% reduction compared to 14.5% for placebo.
- Clinically meaningful itch relief (≥4-point reduction in WI-NRS) was achieved by 66.0% of patients in the 540 mg group, compared to 16.7% in the placebo group.
- Skin clearance (IGA 0/1) was nearly four times higher in the high-dose vixarelimab group than in the placebo group, showing a strong correlation between itch reduction and lesion healing.
- The safety profile was favorable across all doses, with no fatal or serious drug-related treatment-emergent adverse events reported during the double-blind period.
The Clinical Burden of Prurigo Nodularis
Prurigo nodularis (PN) is a chronic, debilitating inflammatory skin disease characterized by the presence of intensely pruritic, symmetric hyperkeratotic nodules. The condition is defined by a vicious itch-scratch cycle that not only causes significant physical trauma to the skin but also results in profound psychological distress, sleep deprivation, and a severely diminished quality of life. The pathophysiology of PN involves a complex interplay between dermal sensory nerves, immune cells (such as T cells, mast cells, and eosinophils), and keratinocytes, collectively referred to as the neuro-immune axis.
Current management strategies often include high-potency topical corticosteroids, phototherapy, and systemic immunosuppressants. While the recent approval of IL-4Rα inhibitors has improved outcomes, a significant portion of the patient population remains refractory to treatment or continues to experience residual itch and nodular burden. There is an urgent clinical need for targeted therapies that address the specific molecular drivers of PN-associated pruritus and skin remodeling.
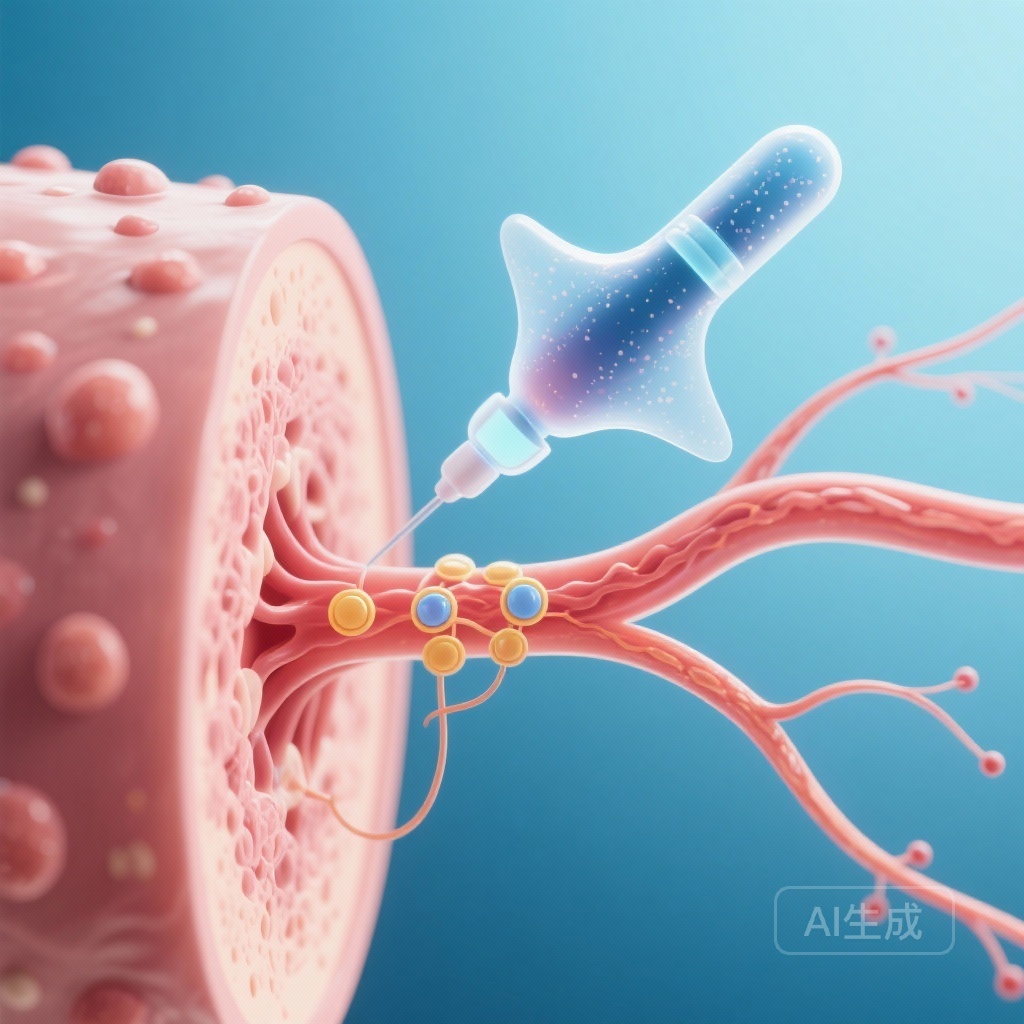
Mechanism of Action: Targeting the OSMRβ Pathway
Vixarelimab is a first-in-class human monoclonal antibody that binds to the Oncostatin M Receptor beta (OSMRβ). This receptor is a critical component of the signaling complexes for two key cytokines: Oncostatin M (OSM) and Interleukin-31 (IL-31). Both cytokines are known to play pivotal roles in the pathogenesis of PN. IL-31 is famously dubbed the “itch cytokine” for its direct activation of pruriceptive sensory neurons. OSM, on the other hand, is involved in promoting inflammation, keratinocyte proliferation, and fibrosis—the hallmark processes leading to the formation of the thick, fibrotic nodules seen in PN.
By antagonizing OSMRβ, vixarelimab simultaneously inhibits both IL-31 and OSM signaling. This dual action is hypothesized to be more effective than targeting IL-31 alone, as it addresses both the neural signaling of itch and the structural skin changes (hyperkeratosis and fibrosis) that characterize the disease.
Study Design and Methodology
This Phase 2b, double-blind, placebo-controlled randomized clinical trial (NCT03816891) was conducted at 72 centers across North America, Europe, and Asia. The study enrolled 190 participants (189 of whom received at least one dose) aged 18 to 80 years. Eligible participants had physician-diagnosed PN for at least six months and were experiencing moderate-to-severe pruritus (defined as a WI-NRS score ≥7 or ≥5 depending on the recruitment phase).
Participants were randomized into four treatment arms for a 16-week double-blind (DB) period:
- High-dose: Vixarelimab 540 mg subcutaneously every 4 weeks.
- Mid-dose: Vixarelimab 360 mg subcutaneously every 4 weeks.
- Low-dose: Vixarelimab 120 mg subcutaneously every 4 weeks.
- Placebo: Subcutaneous injections every 4 weeks.
Following the DB period, an open-label extension (OLE) allowed all participants to receive vixarelimab 360 mg every 2 weeks for 36 weeks. The primary endpoint was the percentage change from baseline in the weekly average of the Worst Itch Numeric Rating Scale (WI-NRS) at week 16.
Key Findings: Rapid and Sustained Itch Reduction
The trial met its primary endpoint with high statistical significance. Vixarelimab showed a clear dose-response relationship in itch reduction. By week 16, the mean percentage change in WI-NRS was -56.2% for the 540 mg group, -51.0% for the 360 mg group, and -33.0% for the 120 mg group, compared to a mere -14.5% for the placebo group.
Clinically meaningful pruritus relief, defined as an improvement of at least 4 points on the WI-NRS, was also significantly higher in the vixarelimab arms. In the high-dose group, 66.0% of patients achieved this threshold, and 61.7% achieved it in the mid-dose group. In contrast, only 16.7% of the placebo group reached this level of improvement. Notably, itch reduction began as early as one week after the first dose, suggesting a rapid onset of action that is highly valued by patients suffering from chronic pruritus.
Secondary Outcomes: Lesion Clearance and Quality of Life
The secondary objective of the study was to evaluate the impact of vixarelimab on the physical manifestations of PN. The PN Investigator Global Assessment (PN-IGA) was used to measure lesion clearance. At week 16, 38.3% of the participants in the 540 mg group and 29.8% in the 360 mg group achieved a PN-IGA score of 0 (clear) or 1 (almost clear), compared to 10.4% in the placebo group.
The correlation between itch reduction and nodule healing was evident; as the pruritus subsided, patients scratched less, allowing the hyperkeratotic nodules to flatten and resolve. This suggests that vixarelimab not only interrupts the neural sensation of itch but also facilitates the reversal of the chronic skin remodeling associated with PN.
Safety and Tolerability Profile
Vixarelimab was generally well-tolerated across the 16-week DB period. The incidence of treatment-emergent adverse events (TEAEs) was similar between the vixarelimab and placebo groups. Most TEAEs were mild to moderate in severity. Importantly, no fatal or serious drug-related TEAEs were reported. The most common adverse events included nasopharyngitis and upper respiratory tract infections, which are typical for biologic therapies targeting immune pathways. No specific signals for conjunctivitis—a common side effect of IL-4Rα inhibitors—were prominently noted in the study data, potentially offering a safety advantage for certain patient subsets.
Expert Commentary
The results of this Phase 2b trial are highly encouraging for the dermatology community. By targeting the OSMRβ pathway, vixarelimab addresses a broader spectrum of the PN pathophysiology than existing therapies that focus solely on TH2 inflammation. The dose-dependent nature of the response provides clinicians with a clear understanding of the drug’s efficacy profile, suggesting that higher doses may be necessary to achieve the best clinical outcomes in terms of both itch and lesion clearance.
However, as with any Phase 2 trial, there are limitations. The study duration of 16 weeks for the primary endpoint, while standard, does not fully capture the long-term sustainability of the response or the potential for complete nodular resolution, which often takes longer than the reduction of itch. Furthermore, while the safety data is promising, larger Phase 3 trials are required to confirm the long-term safety and to detect rarer adverse events. The upcoming Phase 3 program will be pivotal in determining vixarelimab’s place in the treatment paradigm for Prurigo Nodularis.
Conclusion
In conclusion, vixarelimab represents a significant advancement in the targeted treatment of Prurigo Nodularis. By inhibiting the OSMRβ pathway, it provides rapid and substantial relief from the primary symptom—intense pruritus—and promotes the clearing of nodular lesions. With its favorable safety profile and robust efficacy data, vixarelimab is a promising candidate for patients who have failed traditional therapies, potentially redefining the standard of care for this challenging condition.
Funding and ClinicalTrials.gov
This study was funded by Kiniksa Pharmaceuticals, Ltd. The trial is registered at ClinicalTrials.gov with the identifier NCT03816891.
References
- Ständer S, Yosipovitch G, Sofen H, et al. Vixarelimab in Patients With Prurigo Nodularis: A Randomized Clinical Trial. JAMA Dermatol. Published online December 17, 2025. doi:10.1001/jamadermatol.2025.4950.
- Yosipovitch G, et al. Prurigo Nodularis: Pathophysiology and Management. J Am Acad Dermatol. 2020;83(6):1557-1565.
- Nattkemper LA, et al. The Molecular Fingerprint of Prurigo Nodularis and Psoriasis. J Invest Dermatol. 2018;138(8):1729-1737.