High-Level Highlights
Echocardiographic Parity
Both Transcatheter Aortic Valve Implantation (TAVI) and Surgical Aortic Valve Replacement (SAVR) achieved excellent outcomes with remarkably low rates (less than 1%) of moderate or greater paravalvular regurgitation.
Hemodynamic Trade-offs
SAVR was associated with lower mean transprosthetic gradients and larger aortic valve areas compared to TAVI at 30 days, leading to more pronounced regression of left ventricular hypertrophy (LVH) at one year.
Right Ventricular Preservation
TAVI demonstrated a clear advantage in right ventricular (RV) function, with significantly lower rates of RV systolic dysfunction (14.5% vs. 40.7%) and better evolution of overall cardiac damage stage compared to surgery.
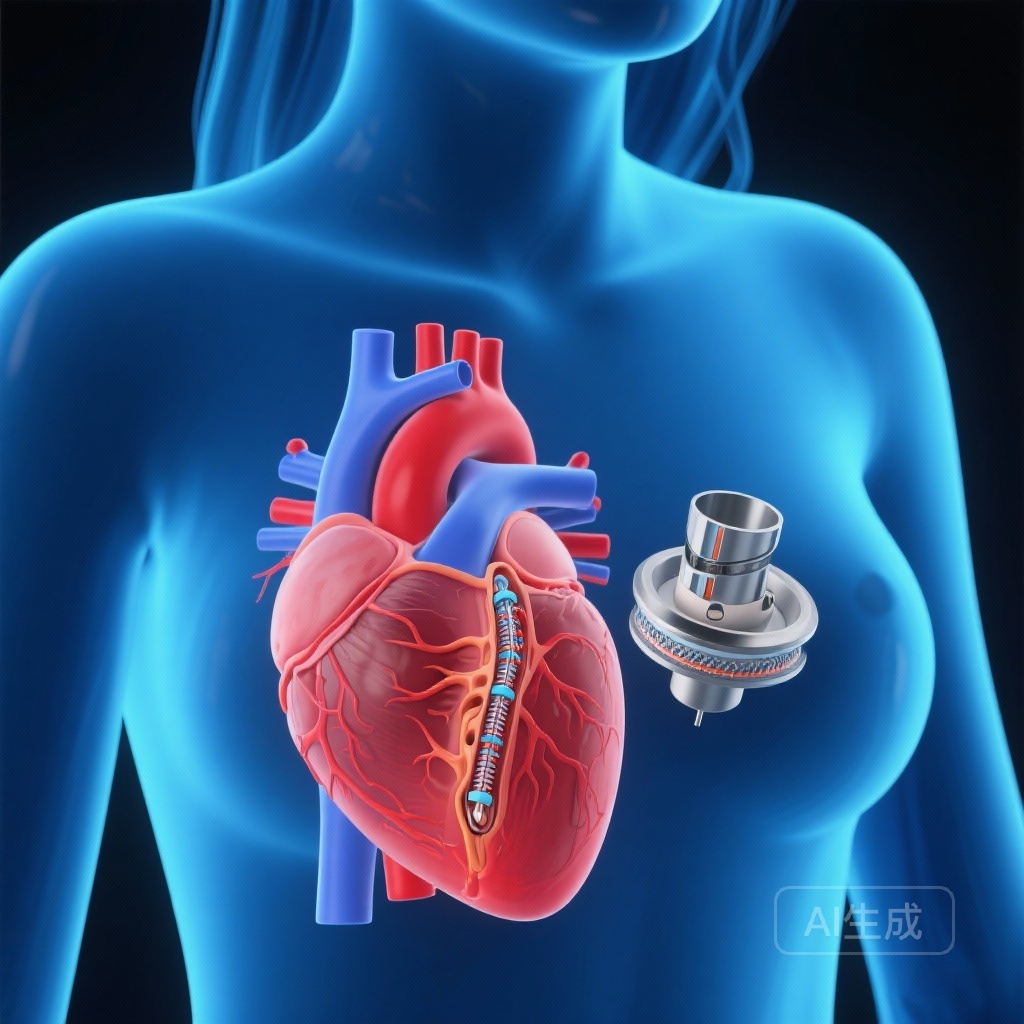
Background: The Gender Gap in Aortic Stenosis Care
Severe aortic stenosis (AS) in women presents unique clinical and anatomical challenges. Historically, women have been underrepresented in major cardiovascular trials, despite the fact that they often present with different phenotypes than men, including smaller aortic annuli, higher rates of left ventricular (LV) concentric remodeling, and increased risk of patient-prosthesis mismatch (PPM) following surgery. The RHEIA (Randomized Research in Women All Comers With Aortic Stenosis) trial was specifically designed to address these disparities. While the primary trial results indicated that TAVI was superior to SAVR regarding the clinical composite of death, stroke, or rehospitalization at one year, understanding the structural and functional changes in the heart—as captured by echocardiography—is essential for long-term management and clinical decision-making.
Study Design and Methodology
The RHEIA trial was a prospective, randomized, controlled trial conducted across 48 centers in Europe. It enrolled 443 women with severe symptomatic AS who were randomized 1:1 to receive either TAVI or SAVR. This specific substudy focused on the echocardiographic outcomes of 356 patients whose imaging was analyzed by an independent core laboratory. The objective was to compare valve hemodynamics, ventricular remodeling, and the progression of cardiac damage between the two intervention groups over a one-year follow-up period. The inclusion of a core laboratory ensures that the findings are standardized and minimizes the inter-observer variability often found in multi-center echocardiographic studies.
Valve Hemodynamics: Gradients and Valve Area
At the 30-day mark, the study revealed notable differences in valve performance. Patients in the SAVR group exhibited lower mean transprosthetic gradients and larger indexed effective orifice areas (EOA) compared to those in the TAVI group. Specifically, TAVI was associated with a higher mean gradient, which likely reflects the anatomical constraints of placing a transcatheter frame within the female aortic root.
However, it is critical to note that despite these higher gradients in the TAVI group, the incidence of severe patient-prosthesis mismatch was low and nearly identical between the two groups (3.0% for TAVI vs. 2.6% for SAVR; P=1). This suggests that even with slightly higher gradients, the hemodynamic performance of modern transcatheter valves in women is clinically sufficient. Furthermore, these hemodynamic parameters remained stable through the one-year follow-up, indicating good short-term durability for both treatment modalities.
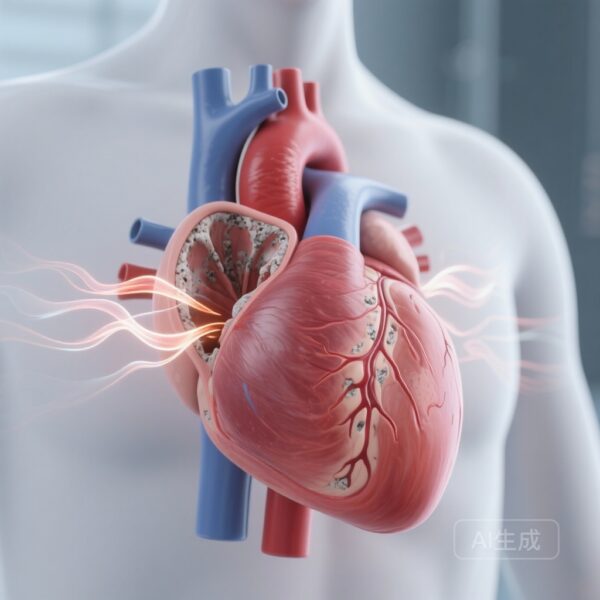
The Myocardial Response: LVH Regression and RV Function
One of the most striking findings of the RHEIA echocardiographic substudy pertains to myocardial remodeling. Left ventricular hypertrophy (LVH) is a common compensatory mechanism in chronic AS, but its persistence after valve replacement is linked to poorer long-term outcomes. The study found that SAVR was more effective at inducing LVH regression. At one year, the rate of residual LVH was 28.6% in the SAVR group compared to 45.3% in the TAVI group (P=0.004). This difference is likely a direct consequence of the lower gradients and larger valve areas achieved through surgical replacement.
Conversely, TAVI showed a significant advantage in preserving right ventricular (RV) function. Post-operative RV dysfunction is a known complication of cardiac surgery, often attributed to the opening of the pericardium, cardiopulmonary bypass, and intraoperative myocardial protection strategies. In the RHEIA trial, RV systolic dysfunction at one year was observed in 40.7% of the SAVR group, compared to only 14.5% in the TAVI group (P<0.001). This suggests that the less invasive nature of TAVI is highly beneficial for maintaining right-sided heart health, which is an increasingly recognized predictor of mortality and quality of life.
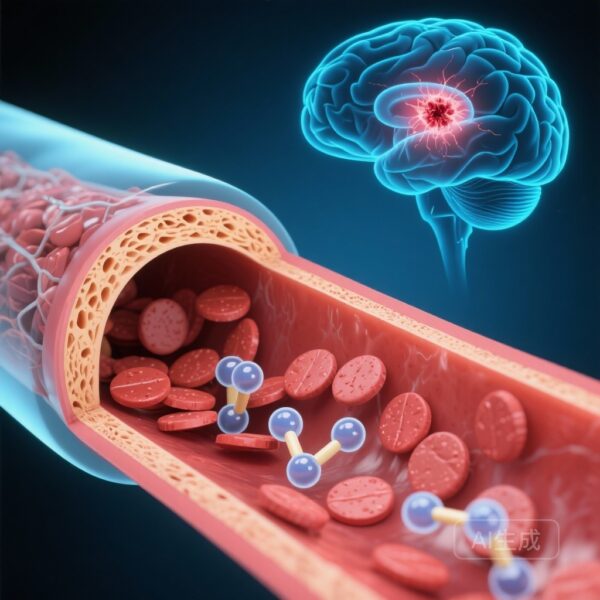
Staging Cardiac Damage: A Global Perspective
The substudy also utilized the Genereux staging classification to evaluate the evolution of cardiac damage. This system categorizes patients based on the extent of damage beyond the aortic valve, including LV involvement (Stage 1), left atrial or mitral valve involvement (Stage 2), pulmonary hypertension or tricuspid valve involvement (Stage 3), and RV dysfunction (Stage 4).
At one year, TAVI patients showed a more favorable evolution of cardiac damage. While the percentage of patients who improved was similar (21.8% for TAVI vs. 18.1% for SAVR), there was a stark difference in those who worsened. Only 16.8% of TAVI patients saw their cardiac damage stage worsen, compared to 47.0% of SAVR patients (P=0.001). This deterioration in the SAVR group was largely driven by the aforementioned decline in RV function.
Expert Commentary and Clinical Implications
The RHEIA trial substudy provides a nuanced view of the ‘price’ of each procedure. For women with severe AS, the choice between TAVI and SAVR may involve a trade-off between left-sided and right-sided benefits. If the primary clinical goal is the aggressive reduction of LV mass and the achievement of the lowest possible gradients, SAVR remains a compelling option, especially in younger women who may benefit from maximized LV remodeling over decades.
However, the high incidence of RV dysfunction and the overall worsening of cardiac damage stages in the surgical arm cannot be ignored. For many women, particularly those who may already have baseline RV strain or those who wish to avoid the systemic trauma of open-heart surgery, TAVI offers a superior profile for preserving global cardiac staging. The low rate of paravalvular regurgitation in the TAVI group—traditionally a concern in transcatheter trials—highlights the technical advancements in valve design and the expertise of contemporary operators.
Summary of Findings
In conclusion, both TAVI and SAVR provide excellent hemodynamic results for women with severe aortic stenosis. The RHEIA trial substudy clarifies that while SAVR excels in gradient reduction and LVH regression, TAVI is significantly more protective of right ventricular function and prevents the progression of multi-chamber cardiac damage. These findings empower clinicians to move toward a more personalized approach to valve selection, weighing the structural benefits of surgery against the functional preservation offered by transcatheter intervention.
Funding and Registration
This research was supported by the RHEIA Trial Investigators and various institutional grants.
ClinicalTrials.gov Identifier: NCT04160130.
References
1. Silva I, Alperi A, Hecht S, et al. Echocardiographic Results of Transcatheter Versus Surgical Aortic Valve Replacement in Women With Severe Aortic Stenosis: The RHEIA Trial. J Am Heart Assoc. 2026;15(1):e047196.
2. Tchétché D, et al. Transcatheter versus surgical aortic valve replacement in women with severe aortic stenosis: the RHEIA trial. Lancet. 2024 (Primary Trial Publication).
3. Genereux P, et al. Staging classification of aortic stenosis based on the extent of cardiac damage: incidence, predictors, and prognostic value. Eur Heart J. 2017;38(45):3351-3358.
4. Vahanian A, et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2022;43(7):561-632.