Highlights
– Achieving very low levels of low-density lipoprotein cholesterol (LDL-C), specifically below 40 mg/dL, is associated with a significant reduction in recurrent major adverse cardiovascular events (MACE) and ischemic stroke.
– The relationship between achieved LDL-C and cardiovascular risk reduction is monotonic, meaning lower levels consistently correlate with better outcomes down to at least 20 mg/dL.
– Long-term safety data from a median follow-up of over 7 years indicate no increased risk of hemorrhagic stroke or other major safety concerns with ultra-low LDL-C levels.
– These findings provide robust evidence for clinicians to pursue intensive lipid-lowering therapy in high-risk patients with a history of ischemic stroke.
Introduction: The Evolution of Lipid Management in Stroke
For decades, the management of low-density lipoprotein cholesterol (LDL-C) has been a cornerstone of secondary prevention in patients with atherosclerotic cardiovascular disease (ASCVD). However, for patients with a history of ischemic stroke, the optimal target for LDL-C reduction has been a subject of intense debate. While the SPARCL trial (Stroke Prevention by Aggressive Reduction in Cholesterol Levels) established the benefit of high-intensity statin therapy, concerns persisted regarding the potential for increased hemorrhagic stroke risk at very low cholesterol levels.
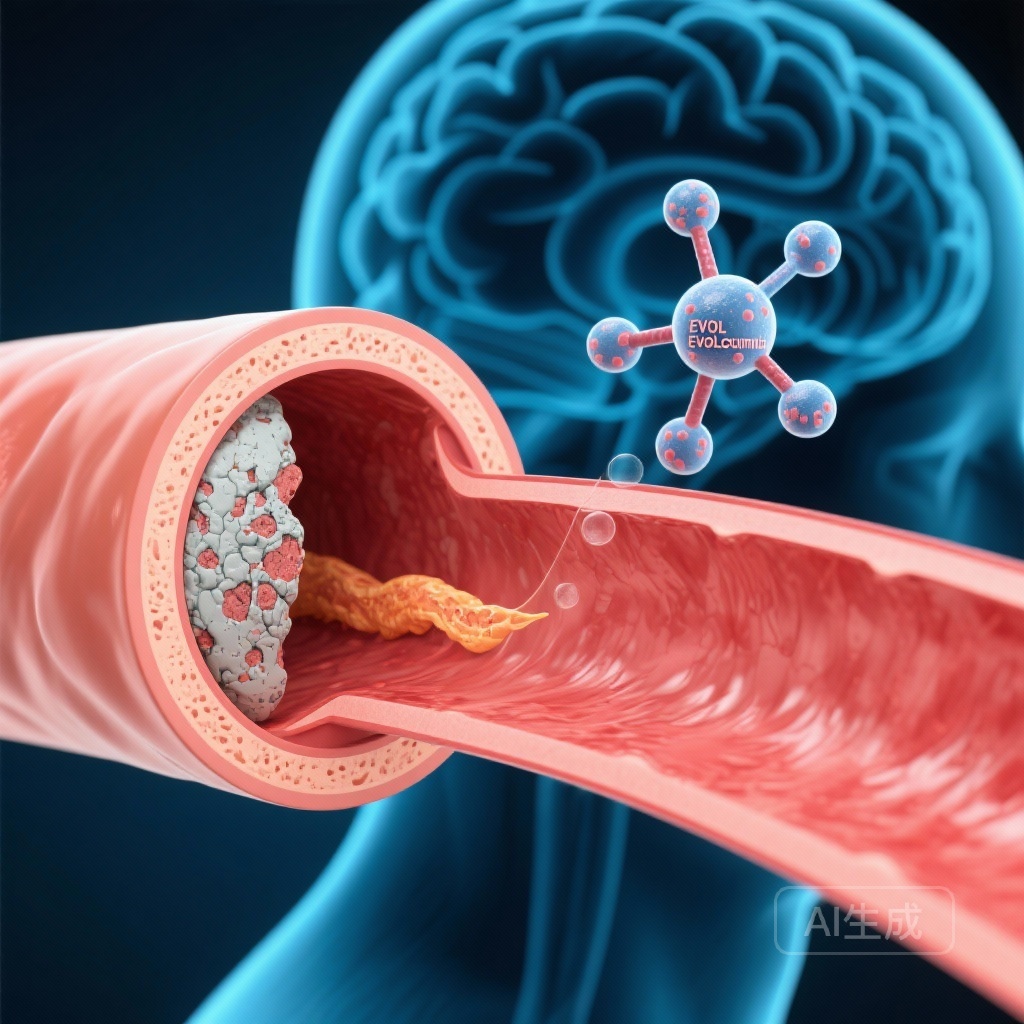
As therapeutic options have expanded to include non-statin therapies like ezetimibe and PCSK9 inhibitors, it has become possible to reach LDL-C levels previously thought unattainable. The question remains: is there a floor to the clinical benefit, or does the ‘lower is better’ hypothesis hold true even at levels below 40 mg/dL? This latest analysis of the FOURIER and FOURIER-OLE trials provides much-needed clarity for the neurology and cardiology communities.
The FOURIER and FOURIER-OLE Analysis: Study Design and Population
This study represents a comprehensive analysis of patients with a history of ischemic stroke who were enrolled in the FOURIER (Further Cardiovascular Outcomes Research With PCSK9 Inhibition in Subjects With Elevated Risk) trial and its subsequent open-label extension, FOURIER-OLE. The original FOURIER trial was a randomized, double-blind, placebo-controlled study evaluating the efficacy of evolocumab, a monoclonal antibody targeting PCSK9, in patients with stable ASCVD already receiving statin therapy.
The analysis focused on 5,291 patients who had a documented ischemic stroke occurring more than four weeks prior to enrollment. The median follow-up in the primary trial was 2.2 years, which was extended by an additional median of 5 years in the OLE phase, providing a robust window to observe long-term safety and efficacy. Patients were categorized based on their achieved LDL-C levels: <20 mg/dL, 20 to <40 mg/dL, 40 to <55 mg/dL, 55 to <70 mg/dL, and ≥70 mg/dL.
Key Findings: A Monotonic Relationship Between LDL-C and Risk Reduction
The results of the analysis demonstrate a clear and consistent benefit to intensive LDL-C lowering. Among the 5,291 patients, the distribution of achieved LDL-C was broad, with over 12% reaching levels below 20 mg/dL and nearly 40% remaining at or above 70 mg/dL.
Primary Outcomes and MACE
The incidence of the primary composite end point—consisting of cardiovascular death, myocardial infarction, stroke, or hospitalization for unstable angina or coronary revascularization—showed a significant monotonic decrease as achieved LDL-C levels declined (Ptrend < 0.001). When compared to patients with an LDL-C ≥70 mg/dL, those who achieved levels <40 mg/dL experienced a 31% reduction in the risk of MACE (Incidence Rate Ratio [IRR], 0.69; 95% CI, 0.57-0.84).
Stroke-Specific Outcomes
Similar trends were observed for stroke-specific endpoints. The risk of all-cause stroke and ischemic stroke both decreased significantly with lower LDL-C levels (Ptrend = 0.002 for both). For patients achieving LDL-C <40 mg/dL, the risk reduction for all stroke was 27% (IRR, 0.73; 95% CI, 0.53-0.99) and for ischemic stroke was 25% (IRR, 0.75; 95% CI, 0.54-1.05) compared to the group with LDL-C ≥70 mg/dL.
Safety Profile: Addressing the Hemorrhagic Stroke Concern
One of the most critical aspects of this study was the evaluation of safety, particularly regarding hemorrhagic stroke. Historical data, primarily from observational studies and a subgroup analysis of the SPARCL trial, had suggested a potential association between very low LDL-C or statin use and an increased risk of intracranial hemorrhage.
However, in this large-scale analysis with extended follow-up, hemorrhagic strokes were infrequent across all groups. Crucially, there was no relationship between the achieved LDL-C level and the incidence of hemorrhagic stroke (Ptrend = 0.85). This finding is consistent with other major PCSK9 inhibitor trials and meta-analyses, suggesting that the feared ‘J-shaped curve’ for LDL-C and stroke risk may be more related to baseline patient characteristics or specific comorbidities rather than the absolute level of cholesterol itself.
Expert Commentary: Clinical Implications and Pathophysiology
These findings reinforce the current shift in international guidelines toward more aggressive lipid management in very high-risk patients. The European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS) currently recommend an LDL-C target of <55 mg/dL for secondary prevention in ASCVD, with an even lower target of <40 mg/dL for patients who experience a second vascular event within two years while on maximally tolerated statin therapy.
From a mechanistic perspective, the benefits of very low LDL-C are likely driven by plaque stabilization and regression. Intensive lowering of LDL-C reduces the lipid core of atherosclerotic plaques, thickens the fibrous cap, and decreases local inflammation within the vessel wall. In the cerebrovascular bed, this translates to a lower risk of thromboembolic events originating from the carotid arteries or the aortic arch, as well as reduced progression of small vessel disease.
While the data are compelling, clinicians must still personalize treatment. The patients in FOURIER had stable ASCVD; therefore, the results may not be directly generalizable to patients with acute stroke or those with specific etiologies like vasculitis or non-atherosclerotic arteriopathies. Furthermore, while the safety profile is reassuring, the high cost of PCSK9 inhibitors remains a barrier to implementation in many healthcare systems, necessitating a focus on high-risk populations who stand to gain the most from these therapies.
Conclusion: Re-evaluating Secondary Prevention Targets
The analysis of the FOURIER and FOURIER-OLE trials provides high-quality evidence that for patients with a history of ischemic stroke, ‘lower is better’ remains the guiding principle for LDL-C management. Achieving levels below 40 mg/dL, and even below 20 mg/dL, offers incremental protection against recurrent ischemic events without compromising safety regarding hemorrhagic stroke. As we move forward, these data support the use of intensive combination therapy—including statins, ezetimibe, and PCSK9 inhibitors—to reach these ambitious but highly beneficial targets.
Funding and ClinicalTrials.gov
The FOURIER and FOURIER-OLE trials were funded by Amgen. The primary trial is registered at ClinicalTrials.gov with the unique identifier: NCT01764633.
References
1. Monguillon V, Kelly PJ, O’Donoghue ML, et al. Efficacy and Safety of Very Low Achieved LDL Cholesterol in Patients With Previous Ischemic Stroke. Circulation. 2026;153(2):86-93. doi:10.1161/CIRCULATIONAHA.125.077549.
2. Sabatine MS, Giugliano RP, Keech AC, et al. Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease. N Engl J Med. 2017;376(18):1713-1722. doi:10.1056/NEJMoa1615664.
3. Amarenco P, Bogousslavsky J, Callahan A 3rd, et al. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006;355(6):549-559. doi:10.1056/NEJMoa061894.
4. Giugliano RP, Pedersen TR, Park JG, et al. Clinical efficacy and safety of achieving very low low-density lipoprotein cholesterol concentrations with the PCSK9 inhibitor evolocumab: a prespecified secondary analysis of the FOURIER outcomes trial. Lancet. 2017;390(10106):1962-1971. doi:10.1016/S0140-6736(17)32290-0.