Posted inInfectious Diseases news Public Health
2024-2025 COVID-19 Vaccines Provide 79% Protection Against Critical Illness Despite Viral Evolution
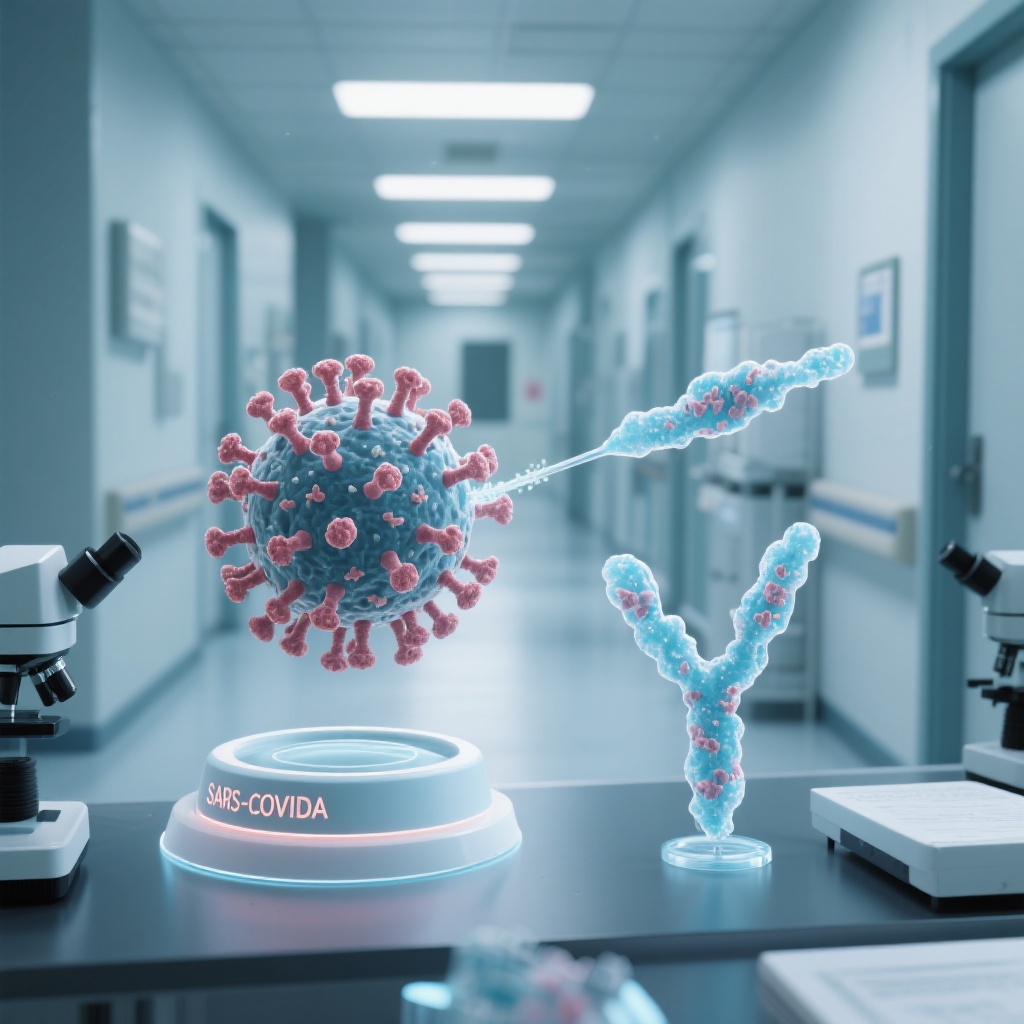
A multicenter study reveals that 2024-2025 COVID-19 vaccines offer 40% protection against hospitalization and 79% against critical illness or death, maintaining efficacy against emerging JN.1 descendants like KP.3.1.1 and XEC.