Highlights
- The combination of sapacitabine and olaparib achieved an objective response rate (ORR) of 50% in patients with germline BRCA1/2-mutated, HER2-negative metastatic breast cancer.
- The median progression-free survival (mPFS) was 9.7 months, with some patients exhibiting exceptional durability exceeding 40 months.
- Hematological toxicities were the primary dose-limiting factor, preventing the determination of a recommended phase 2 dose (RP2D) under the studied schedule.
- Circulating tumor DNA (ctDNA) analysis identified BRCA reversion mutations and microhomology-mediated end-joining (MMEJ) signatures as key drivers of acquired resistance.
Background and Clinical Rationale
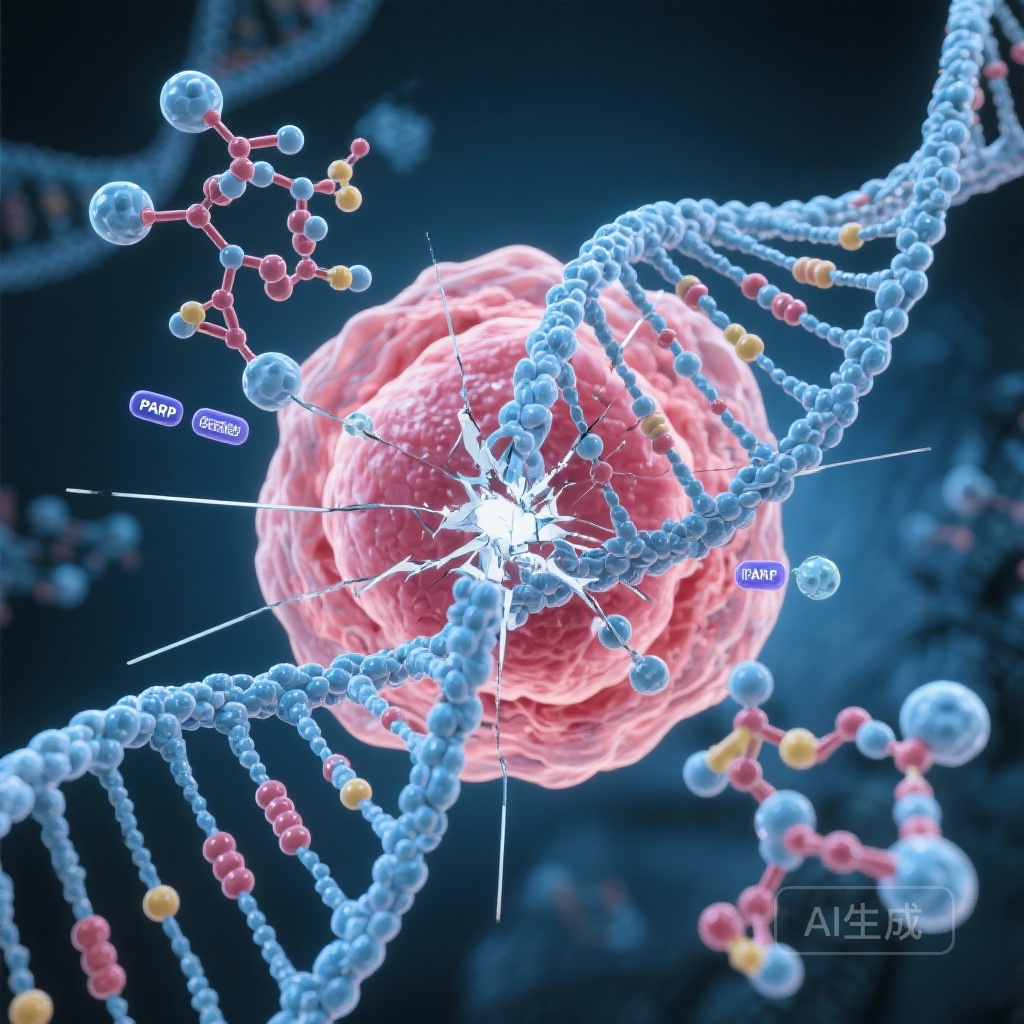
Poly(ADP-ribose) polymerase (PARP) inhibitors have transformed the treatment landscape for patients with germline BRCA1/2 (gBRCA1/2) mutations. However, despite initial efficacy, many patients eventually develop resistance, frequently through the restoration of homologous recombination repair (HRR) or the stabilization of replication forks. To overcome these challenges, researchers are investigating combinatorial strategies that enhance the induction of DNA damage or exploit vulnerabilities in the DNA repair pathway.
Sapacitabine is an orally bioavailable prodrug of CNDAC (2′-C-cyano-2′-deoxy-1-β-D-arabino-pentofuranosylcytosine), a deoxycytidine analog. Unlike traditional antimetabolites, CNDAC incorporates into DNA and induces single-strand breaks (SSBs) that are converted into double-strand breaks (DSBs) during the S-phase of the cell cycle. Given that PARP inhibitors also lead to the accumulation of SSBs and trap PARP proteins on DNA, the combination of sapacitabine and olaparib was hypothesized to act synergistically, overwhelming the repair capacity of HRR-deficient tumor cells.
Study Design and Methodology
This phase Ib investigator-sponsored study (NCT02029001) enrolled patients with gBRCA1/2-mutated, HER2-negative metastatic breast cancer (MBC) who were PARP inhibitor-naive. The primary objective was to determine the recommended phase 2 dose (RP2D) of the sapacitabine and olaparib combination.
The study utilized a 3+3 dose-escalation design. Sapacitabine was administered orally twice daily for 7 days of a 21-day cycle, while olaparib was administered twice daily continuously. Secondary objectives included the assessment of safety, ORR, and mPFS. Translational components involved immunohistochemistry (IHC) on archival tumor tissue for biomarkers of HRR deficiency and replication stress, as well as longitudinal ctDNA monitoring to identify mechanisms of resistance.
Key Findings: Efficacy and Durability
Ten patients were enrolled in the study, consisting of three with BRCA1 mutations and seven with BRCA2 mutations. Despite the small cohort size and the challenges associated with dose escalation, the clinical activity was notable:
Objective Response and Survival
The ORR was 50% (95% CI: 18.7% – 81.3%), with five out of ten patients achieving a confirmed response. The median progression-free survival (mPFS) reached 9.7 months (95% CI: 8.02 – NA). These figures are particularly encouraging given the heavily pretreated nature of the patient population.
Exceptional Responders
The study highlighted significant durability in a subset of patients. Three participants experienced a clinical benefit lasting more than 15 months. Most notably, two patients remained on the trial for over 40 months, suggesting that for certain biological profiles, the combination can induce long-term disease control.
Safety and Tolerability: The Hematologic Bottleneck
The primary hurdle encountered during the study was the significant hematological toxicity. The RP2D could not be established because patients experienced high rates of Grade 3 and 4 neutropenia and thrombocytopenia. These toxicities are consistent with the known side-effect profiles of both nucleoside analogs and PARP inhibitors, which can have additive myelosuppressive effects when combined.
The investigators concluded that the current dosing schedule (7 days on, 14 days off for sapacitabine) combined with continuous olaparib was not feasible for broad clinical application. This finding emphasizes the need for alternative scheduling or more selective agents to mitigate bone marrow suppression.
Translational Insights: Biomarkers and Resistance Mechanisms
The study provided critical data on the molecular underpinnings of response and resistance. IHC analysis of archival tumors showed that responders tended to have high levels of HRR deficiency and markers of replication stress, reinforcing the synthetic lethal rationale of the combination.
At the time of disease progression, ctDNA analysis was performed on samples from responding patients. In two cases, evidence of BRCA reversion mutations was detected. These mutations restore the open reading frame of the BRCA gene, allowing the tumor to regain HRR proficiency. Furthermore, these reversions were associated with a microhomology-mediated end-joining (MMEJ) signature, a known alternative DNA repair pathway that tumors utilize when HRR is compromised. Three other patients showed putative non-reversion resistance mechanisms, highlighting the heterogeneity of escape pathways in gBRCA-mutated cancers.
Expert Commentary and Clinical Implications
While the hematological toxicity profile represents a setback for this specific regimen, the high response rate and durability observed in this trial cannot be ignored. The 50% ORR and nearly 10-month mPFS suggest that the sapacitabine-olaparib combination is highly potent in the gBRCA-mutated setting.
The clinical path forward likely involves two strategies. First, modifying the schedule of sapacitabine (e.g., further intermittent dosing) might allow for marrow recovery. Second, the emergence of PARP1-selective inhibitors offers a promising alternative. Current PARP inhibitors like olaparib inhibit both PARP1 and PARP2; however, PARP2 inhibition is heavily implicated in hematological toxicity. Utilizing a PARP1-selective agent in combination with sapacitabine could maintain the DNA-damaging synergy while sparing the bone marrow.
Summary and Future Directions
In summary, the phase Ib study of sapacitabine and olaparib in BRCA1/2-mutated MBC demonstrates proof-of-concept for combining nucleoside analogs with PARP inhibition. Although the RP2D was not determined due to myelosuppression, the clinical activity was robust and durable in several patients. Future research should prioritize the use of next-generation, PARP1-selective inhibitors and optimized dosing schedules to translate this synergistic potential into a tolerable and effective clinical therapy.
References
Lynce F, Graham N, Kochupurakkal BS, et al. A phase Ib study of sapacitabine and olaparib in patients with BRCA1/2-mutated metastatic breast cancer. Clin Cancer Res. 2025 Dec 3. doi: 10.1158/1078-0432.CCR-25-0571. PMID: 41335237.