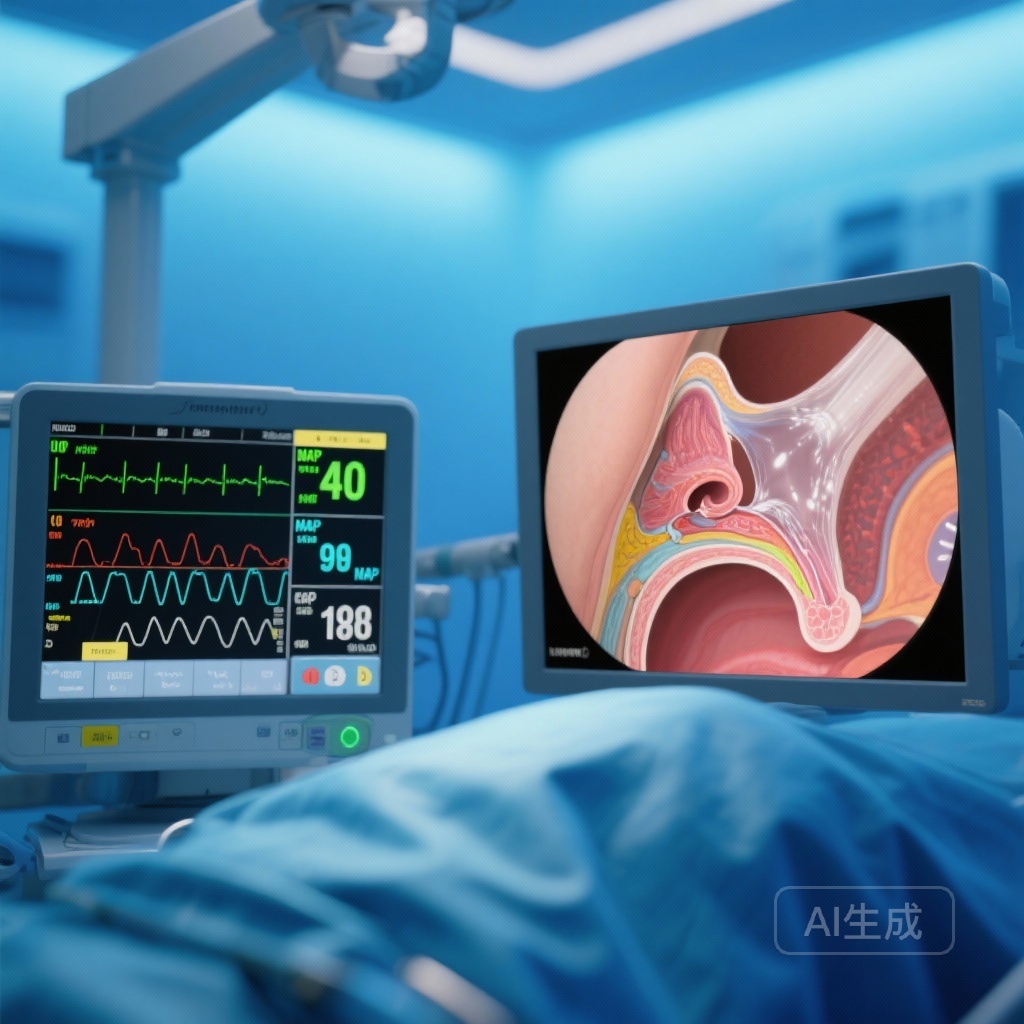
Introduction: The Challenge of Visualization in Rhinosurgery
Endoscopic sinus surgery (ESS) has become the gold standard for treating chronic rhinosinusitis and other sinonasal pathologies. However, the success of ESS is uniquely dependent on the quality of the surgical field. The sinonasal mucosa is highly vascular, and even minor capillary bleeding can significantly impair the surgeon’s view through the endoscope, leading to increased operative time, incomplete disease clearance, and an elevated risk of complications such as orbital injury or cerebrospinal fluid leaks.
To mitigate these risks, anesthesiologists employ ‘controlled hypotension’—the deliberate reduction of systemic blood pressure to maintain a mean arterial pressure (MAP) between 50 and 65 mmHg. While several pharmacological agents are used to achieve this state, there has long been a lack of consensus regarding which drug provides the best balance of surgical visibility, hemodynamic stability, and rapid postoperative recovery. This systematic review and network meta-analysis (NMA) aims to provide a definitive comparison of these agents.
Highlights of the Network Meta-Analysis
Among the various findings of this comprehensive study, three key highlights emerge for clinical practice:
1. Diltiazem, esmolol, and dexmedetomidine are the most effective agents for improving surgical field scores compared to placebo.
2. Dexmedetomidine produces the most profound reduction in mean arterial pressure, though this requires careful monitoring for bradycardia.
3. Esmolol and labetalol provide the added benefit of shortening emergence time, facilitating faster operating room turnover and patient recovery.
Study Design and Methodology
This study followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines to ensure rigorous data synthesis. Researchers conducted an exhaustive search of PubMed, Scopus, Web of Science, and the Cochrane databases through May 2025.
The analysis focused on randomized clinical trials (RCTs) comparing various hypotensive agents—including dexmedetomidine, clonidine, esmolol, labetalol, bisoprolol, metoprolol, diltiazem, nifedipine, and verapamil—against placebo or other active comparators in patients undergoing ESS. A total of 52 RCTs involving 3,526 participants were included, with 43 studies providing sufficient data for the network meta-analysis. The primary outcomes measured were surgical bleeding scores (often utilizing the Boezaart scale), intraoperative MAP, and mean intraoperative heart rate. Secondary outcomes included total blood loss, surgery duration, and the time to emergence from anesthesia.
Key Findings: Comparative Effectiveness of Hypotensive Agents
Improving the Surgical Field
The most critical outcome for the otolaryngologist is the surgical bleeding score. The NMA revealed that several agents significantly outperformed placebo in enhancing visualization. Diltiazem demonstrated the most substantial reduction in bleeding scores (Mean Difference [MD], -1.25; 95% CI, -2.13 to -0.37). It was closely followed by the ultra-short-acting beta-blocker esmolol (MD, -1.16; 95% CI, -1.80 to -0.51) and the alpha-2 agonist dexmedetomidine (MD, -1.09; 95% CI, -1.48 to -0.70). Labetalol and clonidine also showed statistically significant improvements, though to a slightly lesser degree.
Hemodynamic Control: MAP and Heart Rate
Achieving the target MAP is the physiological mechanism behind controlled hypotension. Dexmedetomidine was associated with the most significant reduction in MAP (MD, -30.30 mm Hg), followed by clonidine (-28.61 mm Hg) and esmolol (-27.62 mm Hg). These findings suggest that alpha-2 agonists are particularly potent in their hypotensive effect, likely due to their central sympatholytic action.
Regarding heart rate—a secondary but vital parameter—bisoprolol and verapamil produced the largest reductions at the 60-minute mark. Maintaining a lower heart rate is often as important as lowering blood pressure in ESS, as it reduces the pulsatility of the capillary vessels in the mucosa, further aiding visualization.
Recovery and Emergence Dynamics
A common concern with controlled hypotension is the potential for delayed awakening or ‘hangover’ effects from sedative hypotensives. Interestingly, the study found that esmolol (MD, -3.67 minutes) and labetalol (MD, -3.64 minutes) actually shortened emergence time compared to other protocols. This suggests that the use of these beta-blockers might allow for a reduction in the required dose of volatile or intravenous anesthetics, thereby speeding up the transition to the post-anesthesia care unit (PACU).
Expert Commentary: Mechanistic Insights and Clinical Application
The results of this NMA highlight the nuanced differences between drug classes. The high performance of diltiazem—a calcium channel blocker—is noteworthy. Mechanistically, diltiazem reduces peripheral vascular resistance and myocardial contractility without the profound central sedation associated with alpha-2 agonists. However, its use in many centers is less frequent than esmolol or dexmedetomidine, suggesting a potential shift in protocol might be beneficial for certain patient populations.
Dexmedetomidine remains a favorite for many anesthesiologists because it provides not only hypotension but also analgesia and an ‘opioid-sparing’ effect. However, clinicians must be wary of its tendency to cause prolonged bradycardia and its slower onset/offset compared to esmolol. Esmolol’s rapid titration makes it an ideal choice for ‘on-demand’ hypotension, particularly during the most vascular portions of the surgery, such as the ethmoidectomy or sphenoidotomy.
One limitation noted in the synthesis is the heterogeneity of anesthesia maintenance (e.g., TIVA with propofol vs. volatile agents like sevoflurane), which can independently affect bleeding and recovery. Furthermore, while the GRADE certainty was generally moderate, the varying definitions of ‘surgical field quality’ across 52 trials necessitate a cautious interpretation of the exact mean differences.
Conclusion: Tailoring the Approach to the Patient
The evidence from this systematic review and network meta-analysis confirms that controlled hypotension is a safe and highly effective strategy for optimizing the surgical field in ESS. While several agents are effective, diltiazem and esmolol appear to offer the best balance of visibility and recovery profile. Dexmedetomidine offers superior blood pressure reduction but may be reserved for cases where additional sedation or analgesia is desired.
For the clinical team, the choice of agent should be tailored to the patient’s underlying cardiovascular health and the specific needs of the surgeon. By utilizing these evidence-based pharmacological strategies, surgical teams can ensure better patient outcomes, fewer complications, and more efficient operative workflows.
References
1. Saeed A, et al. Hypotensive Agents for Controlled Hypotension in Endoscopic Sinus Surgery: A Systematic Review and Network Meta-Analysis. JAMA Otolaryngol Head Neck Surg. 2026. doi:10.1001/jamaoto.2025.5222.
2. Boezaart AP, van der Merwe J, Coetzee A. Comparison of sodium nitroprusside- and esmolol-induced controlled hypotension for functional endoscopic sinus surgery. Can J Anaesth. 1995;42(5 Pt 1):373-376.
3. Luier A, et al. Dexmedetomidine vs Remifentanil for Controlled Hypotension in Functional Endoscopic Sinus Surgery: A Meta-analysis. Laryngoscope. 2023.