Introduction: Challenging the Surgical Orthodoxy
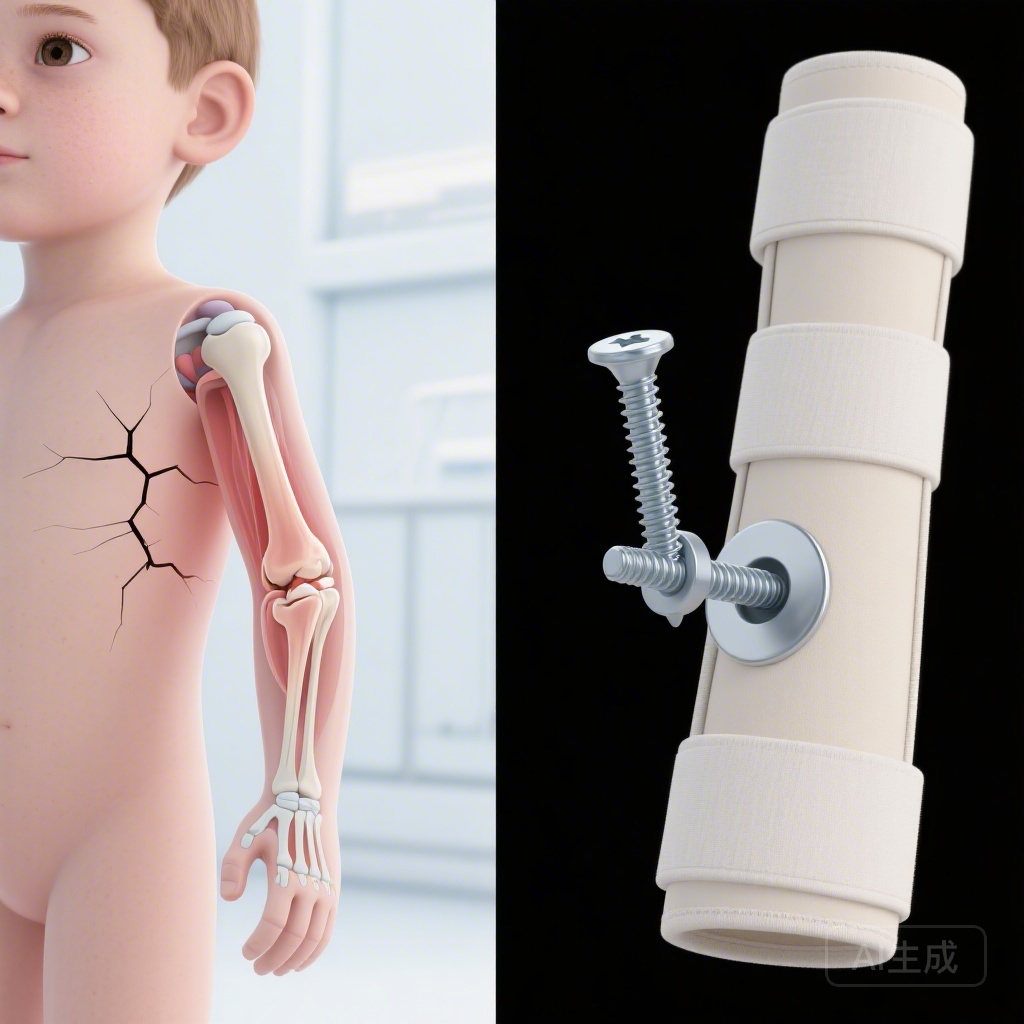
For decades, the management of displaced medial epicondyle fractures in the pediatric population has remained one of the most debated topics in orthopedic trauma. These injuries, which account for approximately 10% to 20% of all pediatric elbow fractures, occur primarily in children aged 7 to 15 years, often during sports or falls where an avulsion force is applied to the medial side of the elbow. Despite their frequency, clinical practice has been deeply divided. On one hand, a growing trend toward surgical fixation has emerged, driven by the intuitive belief that restoring anatomical alignment with screws or wires must yield better functional outcomes. On the other hand, many practitioners have advocated for non-surgical management, citing the elbow’s remarkable capacity for remodeling in children and the inherent risks of anesthesia and surgery.
Until recently, the evidence supporting one approach over the other was largely anecdotal or derived from retrospective cohorts. The SCIENCE study (Surgical fixation versus non-surgical care for children with a displaced medial epicondyle fracture of the elbow) represents a landmark effort to provide high-level, multicentre evidence to resolve this clinical controversy. By evaluating both functional outcomes and economic impacts, this trial offers a definitive perspective on how clinicians should approach these common injuries.
The SCIENCE Trial: Study Design and Methodology
Population and Randomization
The SCIENCE trial was a pragmatic, multicentre, randomized controlled superiority trial conducted across 59 hospitals in the United Kingdom, Australia, and New Zealand. The inclusion criteria targeted children aged 7 to 15 years presenting with a displaced medial epicondyle fracture. To ensure the safety and relevance of the findings, the study excluded patients with incarcerated fragments (where the bone is trapped within the joint), complex fractures extending into the joint, or injuries older than two weeks.
A total of 335 participants were randomly assigned in a 1:1 ratio to either surgical fixation (n=168) or non-surgical care (n=166). Randomization was stratified by clinical centre and the presence of elbow dislocation at the time of injury, ensuring a balanced distribution of baseline characteristics across both arms.
Interventions
The surgical group underwent open reduction and internal fixation (ORIF) under general anesthesia. Surgeons restored the anatomical position of the epicondyle fragment, typically using a compression screw or K-wires. Conversely, the non-surgical group received immobilization of the elbow at approximately 90° of flexion using a cast, splint, or sling. Crucially, both groups were encouraged to begin mobilization as soon as pain allowed, with cast immobilization beyond four weeks discouraged to prevent joint stiffness.
Outcome Measures
The primary endpoint was the Patient Reported Outcomes Measurement System (PROMIS) Upper Extremity Score for Children at 12 months post-randomization. This validated tool assesses the child’s ability to perform daily activities, with higher scores indicating better function. The trial was powered to detect a clinically important difference (MCID) of 4 points. Secondary outcomes included health-related quality of life (EQ-5D-Y), range of motion, and a comprehensive economic evaluation from the perspective of the UK National Health Service (NHS).
Key Findings: Function, Safety, and Economics
Functional Outcomes
The primary analysis included 285 participants who provided 12-month follow-up data. The results were striking in their lack of divergence. At 12 months, the mean PROMIS Upper Extremity score was 54.3 (SD 5.7) in the surgical group and 53.1 (SD 7.8) in the non-surgical group. The mean treatment difference was 1.57 (95% CI -0.01 to 3.14; p=0.052). While the p-value approached the traditional threshold for significance, the effect size remained well below the pre-specified clinical importance threshold of 4 points. This indicates that even if a statistical difference exists, it is too small to be perceived as a benefit by the patients or their families.
Safety and Complications
One of the most compelling arguments for non-surgical care emerged from the safety data. Participants in the surgical group were significantly more likely to undergo additional operations. Among the 150 children who underwent surgery, 14 experienced intraoperative complications (9%), and 7 (5%) required further surgery for postoperative complications. Additionally, 17 participants (11%) underwent a second scheduled operation for the routine removal of metalwork (screws or wires).
In contrast, the non-surgical group demonstrated a much lower complication profile. Only 4 out of 184 participants (2%) experienced complications, with only 3 requiring surgical intervention. This highlights that surgical fixation not only fails to improve function but also introduces a significant burden of avoidable surgical risk and secondary procedures.
Economic Evaluation
The economic analysis was perhaps the most definitive component of the study. Surgical fixation was found to be significantly more expensive, with a mean per-patient cost increase of £2435 compared to non-surgical care. When adjusting for quality-adjusted life years (QALYs), the surgical group actually showed a slight deficit (-0.008 QALYs). Consequently, the probability of surgical fixation being cost-effective at standard willingness-to-pay thresholds (£20,000–£30,000 per QALY) was 0%. From a health policy and resource allocation perspective, surgery for these injuries represents a poor use of public funds.
Expert Commentary and Clinical Implications
The SCIENCE trial provides much-needed clarity for pediatric orthopedic surgeons. For years, the ‘surgical drift’—the gradual shift toward operating on displaced fractures—was fueled by the fear of non-union or long-term joint instability. However, the data now show that even if a non-union occurs in the non-surgical group (which is common in these fractures), it does not translate into functional impairment for the child.
Addressing Dislocation Status
A notable finding of the SCIENCE trial is that the lack of benefit for surgery held true regardless of whether the elbow had been dislocated at the time of injury. Historically, dislocation was often used as a primary justification for surgery, under the assumption that the soft tissue injury was more severe. This trial suggests that the initial dislocation status should not dictate the decision to operate.
Limitations and Generalizability
While the study is robust, it is important to note that it excluded incarcerated fragments. When the medial epicondyle is trapped inside the joint, surgical intervention remains the standard of care to restore joint mechanics. Furthermore, while the 12-month follow-up is sufficient for identifying functional recovery, the ongoing follow-up to age 16 will be crucial for understanding any very long-term effects on joint development or early-onset osteoarthritis.
Conclusion
The SCIENCE trial marks a turning point in the management of pediatric elbow trauma. By demonstrating that surgical fixation offers no clinically relevant functional benefit, increases the risk of complications, and is fundamentally not cost-effective, the study provides a strong evidence base for a ‘non-surgical first’ approach. For the vast majority of children with a displaced medial epicondyle fracture, a simple cast or sling followed by early mobilization is the safest and most efficient path to recovery. Clinicians should now confidently transition away from routine surgical fixation for these injuries, reserving surgery only for specific cases like joint incarceration.
Funding and Clinical Trial Registration
This research was funded by the National Institute for Health and Care Research (NIHR) Health Technology Assessment programme (17/18/02), with additional support from the NIHR Academy, Oxford NIHR Biomedical Research Centre, and the Starship Foundation (New Zealand). The trial is registered with ISRCTN, number ISRCTN16619778.