Highlights
The Pericapsular Nerve Group (PENG) block achieved a significantly higher percentage of summed pain intensity difference (%SPID) compared to the infra-inguinal Fascia Iliaca Block (FIB) during the first hour (62.7% vs. 38.0%).
Significantly more patients in the PENG group reached the clinically meaningful threshold of 50% pain reduction (75% vs. 22%).
There were no significant differences in opioid consumption or adverse events between the two groups, suggesting PENG is a safe and potent alternative for acute pain management.
Introduction: The Challenge of Acute Pain in Hip Fractures
Hip fractures represent a significant burden on global healthcare systems, particularly among the elderly population. Beyond the surgical challenge, the immediate management of acute pain in the emergency department (ED) is a critical determinant of patient outcomes. Severe pain in these patients is associated with delirium, cardiovascular stress, and delayed mobilization, which in turn increases the risk of pneumonia and venous thromboembolism.
Traditional analgesic strategies, primarily systemic opioids, are often limited by side effects such as respiratory depression, sedation, and nausea—complications that are particularly poorly tolerated by geriatric patients. Consequently, regional anesthesia has become a cornerstone of multimodal analgesia. While the Fascia Iliaca Block (FIB) has long been the recommended standard for ED-based pain control, its efficacy can be variable. The recent introduction of the Pericapsular Nerve Group (PENG) block has sparked debate over whether a more targeted anatomical approach could offer superior results.
The Evolution of Regional Anesthesia: From FIB to PENG
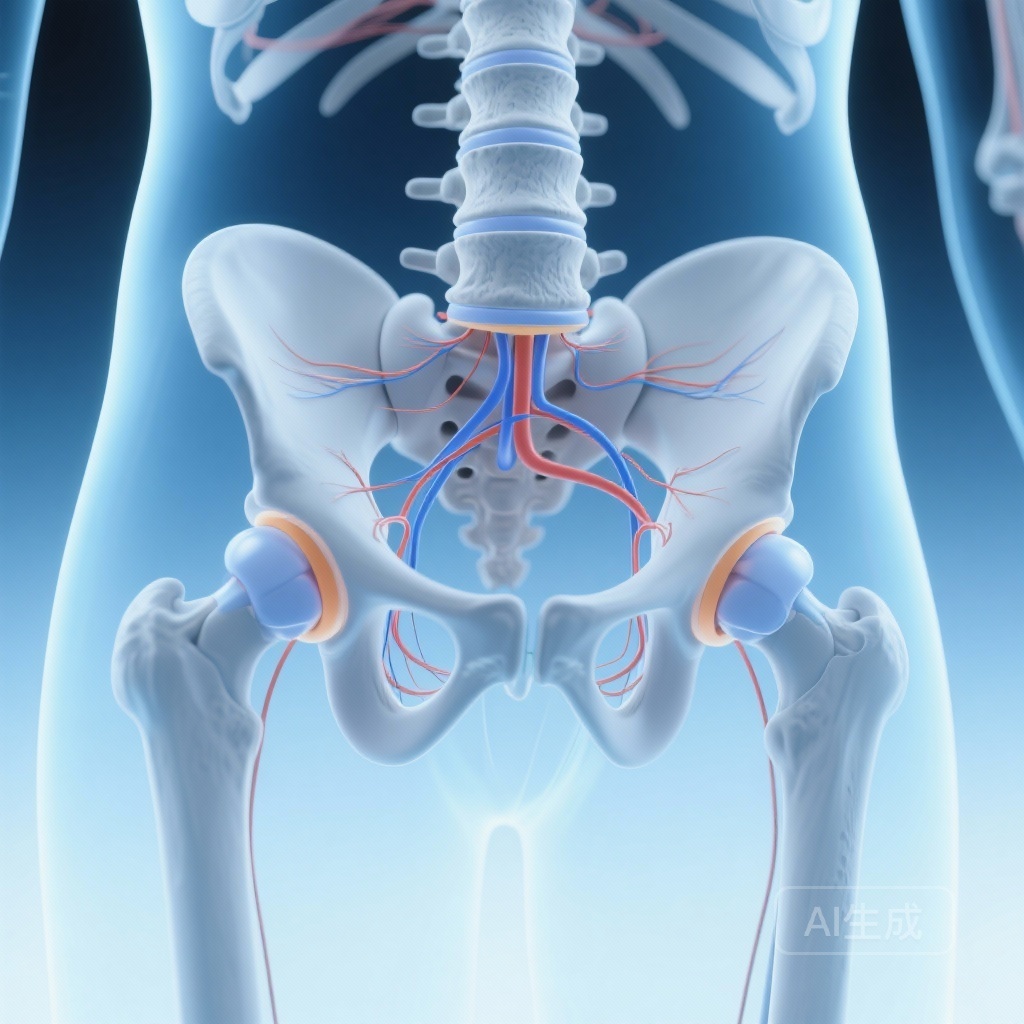
The FIB relies on the volume-based spread of local anesthetic beneath the fascia iliaca to anesthetize the femoral nerve and, ideally, the lateral femoral cutaneous and obturator nerves. However, the obturator nerve is notoriously difficult to reach with an infra-inguinal approach, often leading to incomplete analgesia of the hip joint capsule.
In contrast, the PENG block, first described by Girón-Arango and colleagues in 2018, is designed to target the articular branches of the femoral nerve, the obturator nerve, and the accessory obturator nerve. These branches are located in the space between the psoas tendon anteriorly and the pubic ramus posteriorly. By depositing local anesthetic in this specific osteofascial plane, clinicians can theoretically achieve denser sensory blockade of the anterior hip capsule with lower volumes and higher precision.
Study Design and Methodology
This randomized clinical trial was conducted in an academic emergency department to evaluate the comparative efficacy of PENG and FIB. The study enrolled 64 adult patients (32 per group) presenting with acute hip fractures and reporting at least moderate pain (visual analogue scale [VAS] score ≥ 4).
Intervention Protocols
Patients were randomly allocated to one of two groups:
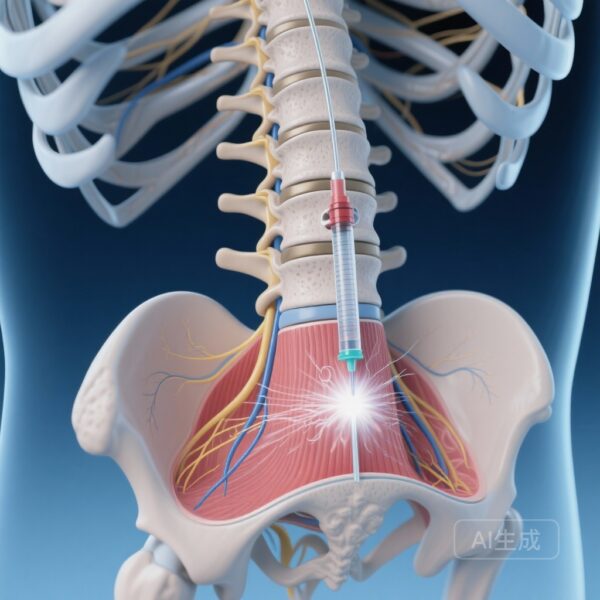
1. PENG Group: Received 20 ml of 0.375% levobupivacaine plus 4 mg of dexamethasone.
2. FIB Group: Received 30 ml of 0.25% levobupivacaine plus 4 mg of dexamethasone.
Both blocks were performed under ultrasound guidance by experienced clinicians. The use of dexamethasone as an adjuvant was standardized across both groups to prolong the duration of the block.
Primary and Secondary Endpoints
The primary outcome was the percentage of summed pain intensity difference (%SPID). This metric is calculated from the VAS scores measured at multiple intervals during the first hour post-block, providing a comprehensive view of the analgesic trajectory rather than a single snapshot. Secondary outcomes included the proportion of ‘responders’ (those reaching 33% and 50% SPID), the amount of rescue opioid administered (morphine milligram equivalents), and the incidence of adverse events such as local anesthetic systemic toxicity (LAST) or nerve injury.
Key Findings: Superiority of the PENG Block
The results of the trial indicate a clear advantage for the PENG block in the immediate acute phase of care.
Pain Intensity Reduction (%SPID)
The PENG group demonstrated a significantly higher %SPID in the first hour compared to the FIB group. The mean %SPID for PENG was 62.7% (95% CI 52.9–72.4%), while the FIB group achieved only 38.0% (95% CI 30.7–45.4%). This difference of 24.7% was statistically significant (p < 0.001), suggesting that PENG provides nearly double the cumulative pain relief of FIB in the critical first hour after intervention.
Clinical Thresholds and Opioid Consumption
The clinical impact was even more evident when looking at responder rates. In the PENG group, 24 out of 32 patients (75%) achieved a 50% reduction in pain intensity, compared to only 7 out of 32 (22%) in the FIB group. Similarly, 87.5% of PENG patients reached the 33% SPID threshold, versus 59.4% in the FIB group (p = 0.022). Interestingly, despite the superior pain scores in the PENG group, the total rescue opioid dose administered within the first hour did not differ significantly between groups, though this may be attributed to the relatively short observation window.
Safety and Adverse Events
Safety is a paramount concern in regional anesthesia. The study reported no significant differences in adverse events. No cases of local anesthetic systemic toxicity, vascular puncture, or persistent neurological deficits were observed in either cohort. This reinforces the safety profile of both ultrasound-guided techniques when performed by trained personnel.
Expert Commentary: Why PENG Outperforms FIB
The findings of Di Pietro et al. align with the anatomical understanding of hip innervation. The anterior hip capsule, where most fracture pain originates, is primarily innervated by the articular branches of the femoral and obturator nerves. The PENG block’s specific targeting of the space between the psoas tendon and the iliopubic eminence allows the anesthetic to pool directly where these sensory branches are most concentrated.
Anatomical Rationale
The FIB often fails to provide adequate obturator nerve blockade because the fascia iliaca is a distal site relative to the nerve’s deep pelvic course. By moving the injection site closer to the hip joint’s sensory supply, the PENG block bypasses the need for large-volume cephalad spread, which is often inconsistent in the elderly due to fascial changes or previous surgeries.
Clinical Implications for the Emergency Department
For ED physicians, the PENG block offers several advantages. First, the higher success rate in achieving substantial pain relief (50% reduction) makes it a more reliable tool for facilitating early radiological imaging and physical examination. Second, because the PENG block is essentially a ‘pericapsular’ injection, it is largely motor-sparing, potentially allowing for better preservation of muscle strength compared to a high-volume FIB, which can cause significant quadriceps weakness.
Study Limitations
While the results are compelling, some limitations must be acknowledged. The study focused on the first hour post-intervention. While the first hour is critical for ED throughput and patient comfort, long-term data on the duration of analgesia and the impact on postoperative recovery or length of hospital stay were not the primary focus. Additionally, the PENG group used a higher concentration of levobupivacaine (0.375% vs. 0.25%), which may have contributed to the density of the block, although the FIB group received a higher total volume.
Conclusion and Summary
The randomized trial by Di Pietro et al. provides high-quality evidence that the PENG block is superior to the infra-inguinal FIB for the acute management of pain in hip fracture patients. With a significantly higher percentage of pain reduction and a higher proportion of patients reaching meaningful analgesic thresholds, the PENG block should be considered a first-line regional anesthetic technique in the emergency department setting. As clinicians continue to seek opioid-sparing strategies for vulnerable populations, the PENG block stands out as a precise, effective, and safe modality that translates anatomical insights into superior clinical care.
References
1. Di Pietro S, Maffeis R, Jannelli E, et al. Comparing the pericapsular nerve group block and fascia iliaca block for acute pain management in patients with hip fracture: a randomised clinical trial. Anaesthesia. 2025;80(12):1484-1492.
2. Girón-Arango L, Peng PWH, Chin KJ, Brull R, Perlas A. Pericapsular Nerve Group (PENG) Block for Hip Fracture. Reg Anesth Pain Med. 2018;43(8):859-863.
3. Guay J, Kopp S. Peripheral nerve blocks for hip fractures in adults. Cochrane Database Syst Rev. 2020;11(11):CD001159.