Highlight
– In a multicenter randomized trial of low‑risk AMI patients who completed 1 month of uneventful DAPT after successful complete revascularization, switching to P2Y12‑inhibitor monotherapy was noninferior to continuing DAPT for a composite of ischemic and major bleeding outcomes at 11 months.
– P2Y12‑inhibitor monotherapy halved clinically relevant bleeding (BARC 2/3/5) compared with continued DAPT (2.6% vs 5.6%; HR 0.46; 95% CI 0.29–0.75), with similar ischemic event rates and rare stent thrombosis.
Background
Dual antiplatelet therapy (DAPT), typically aspirin plus a P2Y12 inhibitor, has been the cornerstone of secondary prevention after percutaneous coronary intervention (PCI) for acute myocardial infarction (AMI). Contemporary drug‑eluting stents (DES), improvements in PCI technique, and better secondary prevention have reduced ischemic complications after PCI, but bleeding remains an important cause of morbidity and a competing risk that can offset ischemic benefit. Optimal DAPT duration after PCI for AMI remains an area of active investigation, particularly the trade‑off between preventing ischemic events and causing bleeding.
Study design
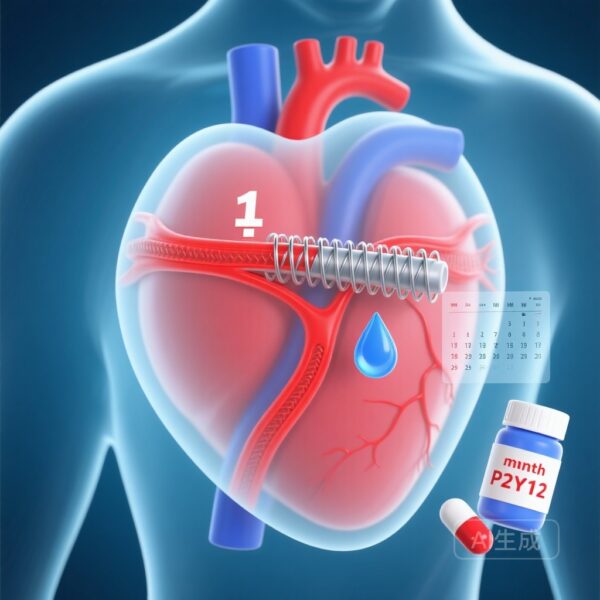
The TARGET‑FIRST trial was a multicenter, open‑label, randomized study conducted at 40 European sites. Adults presenting with AMI who had undergone successful complete revascularization within 7 days and received guideline‑recommended therapy with a contemporary DES were eligible. Patients who completed 1 month of DAPT without ischemic or major bleeding events were randomized to either:
- Transition to P2Y12‑inhibitor monotherapy for the remaining 11 months, or
- Continue DAPT for an additional 11 months (total 12 months).
The primary outcome was a composite of all‑cause death, myocardial infarction, stent thrombosis, stroke, or major bleeding (Bleeding Academic Research Consortium [BARC] type 3 or 5) at 11 months after randomization, tested for noninferiority with a prespecified margin of 1.25 percentage points. The main secondary outcome was clinically relevant bleeding (BARC type 2, 3, or 5) at 11 months, tested for superiority.
Key findings
Enrollment and randomization: Of 2246 enrolled patients, 1942 met randomization criteria and were randomized: 961 to P2Y12‑inhibitor monotherapy and 981 to continued DAPT.
Primary composite outcome
At 11 months after randomization, the primary composite event occurred in 20 patients (2.1%) in the P2Y12‑inhibitor monotherapy group and 21 patients (2.2%) in the continued DAPT group. The between‑group difference was −0.09 percentage points (95% CI, −1.39 to 1.20), meeting the prespecified criterion for noninferiority (P = 0.02 for noninferiority).
Bleeding outcomes
Clinically relevant bleeding (BARC 2, 3, or 5) occurred in 2.6% of patients randomized to P2Y12‑inhibitor monotherapy versus 5.6% in the DAPT arm (hazard ratio [HR] 0.46; 95% CI 0.29–0.75; P = 0.002 for superiority). Major bleeding (BARC 3 or 5) was included in the primary composite but was less frequent than the broader BARC 2/3/5 category; the absolute bleeding reduction was driven primarily by fewer BARC type‑2 events and fewer composite clinically relevant bleeding events overall.
Ischemic events and stent thrombosis
Rates of myocardial infarction, stent thrombosis, stroke, and all‑cause mortality were low and numerically similar between arms. Stent thrombosis was rare and did not differ significantly between groups, reassuring for procedural safety in this selected low‑risk population.
Safety and adverse events
Serious adverse event rates appeared similar between groups. No unexpected safety signals were reported.
Interpretation and clinical implications
TARGET‑FIRST demonstrates that, in a prespecified low‑risk population of AMI patients who had early complete revascularization and an uneventful first month of DAPT, de‑escalation to P2Y12‑inhibitor monotherapy is noninferior for a composite of ischemic and major bleeding outcomes and yields a substantial reduction in clinically relevant bleeding.
Where the data are most applicable
These findings apply to patients matching the trial entry criteria: acute MI with successful and complete revascularization within 7 days, implantation of contemporary DES, and no ischemic or major bleeding events while receiving 1 month of DAPT. The population was overall low risk for recurrent ischemia; extrapolation to patients with high ischemic risk, incomplete revascularization, complex PCI (e.g., left main, multivessel disease not fully revascularized), or early complications should be cautious.
Choice of P2Y12 inhibitor
The trial allocated patients to P2Y12‑inhibitor monotherapy but did not mandate a single agent in the synopsis provided here. Clinical choice between clopidogrel, ticagrelor, or prasugrel should be individualized based on bleeding and ischemic risk, prior tolerance, drug interactions, and guideline recommendations. Prior trials of P2Y12 monotherapy have largely focused on ticagrelor or clopidogrel strategies in different contexts; agent‑specific differences may matter, especially in higher‑risk populations.
Impact on guideline‑minded practice
These results reinforce a growing evidence base supporting shorter DAPT and selective aspirin discontinuation strategies to reduce bleeding without increasing ischemic events in appropriately selected patients. The findings provide a pragmatic option for clinicians treating low‑risk AMI patients who have stable early post‑PCI courses.
Comparison with prior evidence
Previous randomized trials have explored shortened DAPT, P2Y12‑inhibitor monotherapy after a brief DAPT course, or aspirin withdrawal after a variable interval, often in heterogeneous populations. TARGET‑FIRST complements these data by focusing specifically on early complete revascularization and a 1‑month DAPT run‑in for AMI patients. Its observed substantial bleeding reduction mirrors patterns seen in other studies that prioritized bleeding endpoints when aspirin was discontinued early while maintaining a potent P2Y12 agent.
Strengths
- Randomized design with a sizeable sample and pragmatic inclusion of contemporary PCI practice.
- Clear, clinically relevant endpoints including combined ischemic and bleeding outcomes and a prespecified noninferiority margin.
- Low event rates reflecting modern therapy and successful revascularization; clinically meaningful reduction in bleeding.
Limitations and cautions
- Open‑label design — symptomatic bleeding ascertainment or treatment decisions could be influenced by knowledge of assignment, although hard ischemic endpoints are less vulnerable.
- Selected low‑risk population: enrollment required no ischemic or major bleeding events during the first month, and complete revascularization within 7 days. Findings should not be generalized to higher ischemic‑risk AMI patients or those with incomplete revascularization.
- Low absolute event rates — while noninferiority was met, low comp event rates widen uncertainty about rare ischemic outcomes (e.g., stent thrombosis) in broader populations.
- Sponsor support from device manufacturer (MicroPort); although not necessarily introducing bias, it warrants attention to trial conduct and independent replication.
Practical recommendations
For clinicians treating AMI patients who meet the trial’s inclusion characteristics, consider the following approach:
- Ensure guideline‑based revascularization with contemporary DES and optimal secondary prevention.
- After 1 month of uneventful DAPT, consider switching to P2Y12‑inhibitor monotherapy if the patient is low ischemic risk and at increased bleeding risk or when clinician and patient favor bleeding risk reduction.
- Select the specific P2Y12 agent based on patient characteristics — consider a potent agent (ticagrelor/prasugrel) for higher ischemic risk if bleeding is acceptable, or clopidogrel if bleeding risk dominates and CYP2C19 considerations permit.
- Individualize decisions in patients outside the trial population (incomplete revascularization, recent stent thrombosis, complex left main intervention, or concurrent indications for antithrombotic therapy).
Unanswered questions and future research
Key knowledge gaps remain. These include the optimal P2Y12 agent for monotherapy (clopidogrel vs potents), applicability to higher ischemic‑risk AMI cohorts, the role of ischemic risk scores and platelet function/genotype testing to guide personalization, and longer‑term outcomes beyond 12 months. Additional randomized data and pooled analyses will help refine patient selection and agent choice.
Conclusions
TARGET‑FIRST provides high‑quality randomized evidence that, in selected low‑risk AMI patients with early complete revascularization and an uneventful first month of DAPT, switching to P2Y12‑inhibitor monotherapy is a safe and bleeding‑sparing strategy compared with continuing DAPT for 12 months. Clinicians should apply this approach selectively, integrating patients’ ischemic and bleeding risk profiles and considering agent‑specific properties.
Funding and ClinicalTrials.gov
Funded by MicroPort (France). ClinicalTrials.gov number: NCT04753749.
References
1. Tarantini G, Honton B, Paradies V, et al.; TARGET‑FIRST Investigators. Early Discontinuation of Aspirin after PCI in Low‑Risk Acute Myocardial Infarction. N Engl J Med. 2025 Nov 27;393(21):2083‑2094. doi: 10.1056/NEJMoa2508808. PMID: 40888726.
Note: This article interprets the TARGET‑FIRST trial and places it in clinical context. Clinicians should consult full trial publication and current guideline documents when applying these findings to patient care.