High-Level Highlights
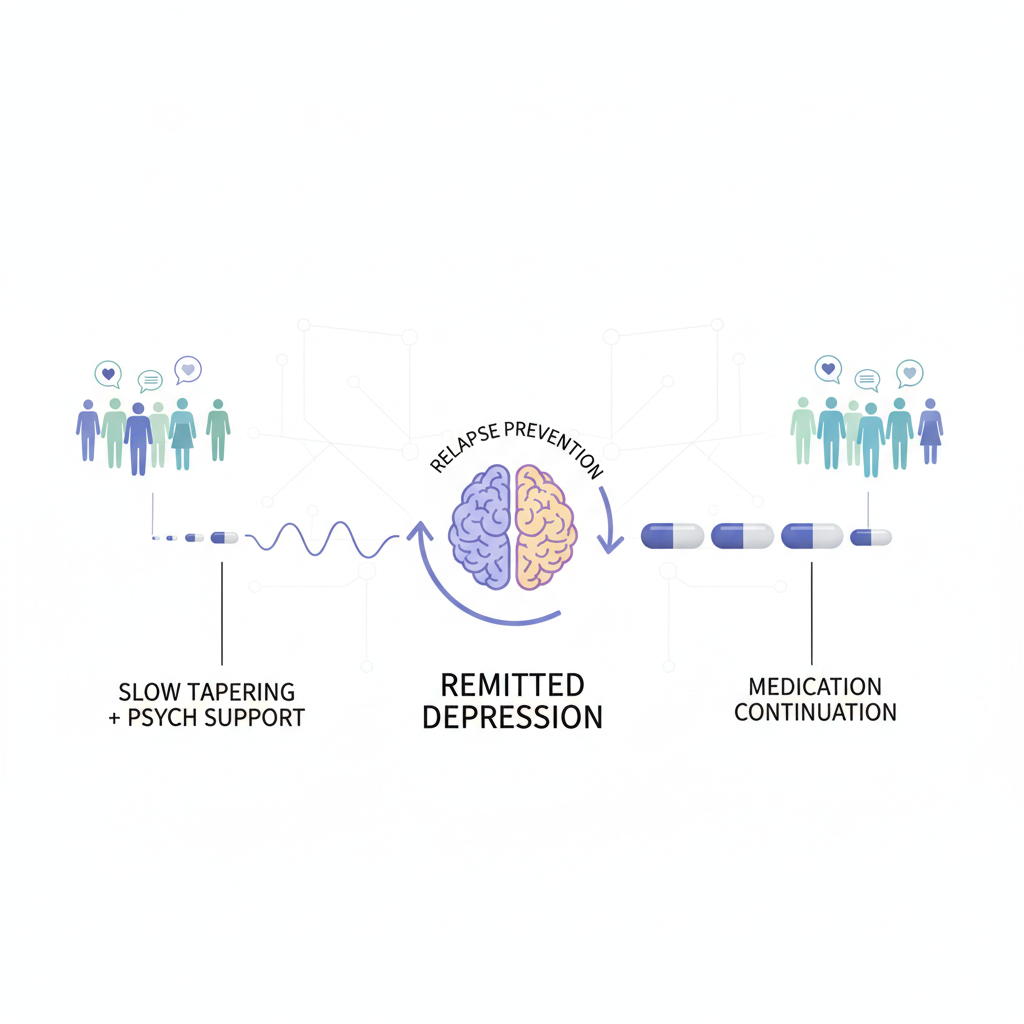
- Slow tapering (>4 weeks) combined with structured psychological support is as effective as continuing standard-dose antidepressants for preventing relapse in remitted depression.
- Abrupt discontinuation and fast tapering (≤4 weeks) are associated with significantly higher relapse risks compared to continuation strategies.
- The Number Needed to Treat (NNT) for slow tapering plus psychological support to match the efficacy of continuation is 5.4, indicating high clinical utility.
- While data for anxiety disorders follow similar trends, the evidence base is currently less robust than for depressive disorders, necessitating cautious clinical application.
The Clinical Challenge: Navigating the End of Antidepressant Therapy
Antidepressants are cornerstones in the management of moderate-to-severe depressive and anxiety disorders. However, a significant clinical dilemma persists: how and when to stop them. While clinical guidelines often recommend continuing medication for 6 to 12 months post-remission to prevent relapse, many patients remain on these medications for years, sometimes without a clear ongoing indication. This long-term use raises concerns regarding overprescribing, cumulative side effects, and the psychological burden of perceived dependency.
The Fear of Relapse vs. The Desire for Discontinuation
The primary barrier to deprescribing is the risk of relapse—the return of depressive symptoms—and the confounding presence of antidepressant withdrawal syndrome. Until recently, clinicians lacked a high-certainty evidence base to determine which tapering strategy minimizes these risks. The study by Zaccoletti and colleagues, published in Lancet Psychiatry, addresses this gap by providing the first comprehensive network meta-analysis (NMA) comparing various deprescribing approaches.
Study Design and Methodology
This systematic review and network meta-analysis utilized data from 76 randomized controlled trials (RCTs) involving 17,379 participants. The researchers conducted an exhaustive search of databases including PubMed, PsycINFO, and trial registries up to April 2025.
Inclusion Criteria and Populations
The analysis focused on adults with fully or partially remitted depressive or anxiety disorders. The mean age of participants was 45.2 years, with a notable majority being female (67.5%). The vast majority of the studies (79%) focused on depression, while 21% addressed anxiety disorders.
Intervention Categories
The NMA compared several distinct strategies:
The primary endpoint was the relapse rate by the end of the trial follow-up, which averaged approximately 46 weeks.
Key Findings: The Superiority of Slow Tapering plus Support
The results of the frequentist network meta-analysis provide a clear hierarchy of efficacy for preventing relapse.
The Most Effective Strategies
The study found that the following approaches significantly outperformed abrupt discontinuation:
Critically, the analysis revealed that slow tapering combined with psychological support was statistically indistinguishable from continuing the medication at a standard dose. This finding is revolutionary, as it suggests that with the right support and timeframe, patients can achieve the same level of stability while off medication as those who stay on it.
The Failure of Rapid Methods
In contrast, fast tapering (≤4 weeks) and abrupt stopping were associated with much higher relapse rates. Fast tapering plus psychological support (RR 0.52, but with a 95% CI of 0.27–1.01) and slow tapering alone (RR 0.81, 95% CI 0.56–1.18) did not show a statistically significant benefit over abrupt discontinuation in terms of relapse prevention. This highlights that the duration of the taper and the addition of psychological interventions are not merely optional extras but essential components of a successful deprescribing plan.
Expert Commentary: Mechanistic Insights and Clinical Nuance
The finding that slow tapering alone was not significantly superior to abrupt stopping—while the addition of psychological support made it highly effective—merits deep clinical reflection.
The Synergy of Psychology and Pharmacology
Psychological support, particularly Cognitive Behavioral Therapy (CBT) or Mindfulness-Based Cognitive Therapy (MBCT), likely provides patients with the emotional regulation tools necessary to distinguish between transient withdrawal symptoms and a true recurrence of depression. Withdrawal symptoms, such as irritability, insomnia, and ‘brain zaps,’ can often be mistaken for a relapse, leading to the premature reinstatement of medication. Structured support helps patients navigate this ‘discontinuation phase’ with greater resilience.
The Anxiety Data Gap
While the results for anxiety disorders were consistent with those for depression in terms of directionality, the researchers noted that the evidence base was smaller. Clinicians should exercise more caution when deprescribing in remitted anxiety, as the certainty of the evidence is currently lower.
Methodological Strengths and Limitations
The study’s strength lies in its use of a network meta-analysis, which allows for the comparison of interventions that have never been tested against each other in head-to-head trials. However, the researchers noted moderate heterogeneity (τ2=0.07). Furthermore, the definition of ‘slow tapering’ as anything over four weeks may still be too rapid for some patients, particularly those on long-term paroxetine or venlafaxine. Recent pharmacological theories suggest ‘hyperbolic’ tapering—reducing doses in smaller and smaller increments as the dose approaches zero—may be even more effective, though this was not specifically isolated in the current NMA.
Conclusion: Implications for Clinical Practice
The Zaccoletti et al. study provides a robust mandate for a shift in how we approach the end of antidepressant treatment. The data suggests that deprescribing is not a simple ‘stop’ command but a clinical process that requires time and therapeutic engagement.
Recommendations for Clinicians
This study effectively removes the ‘trial and error’ approach to deprescribing, replacing it with a data-driven strategy that prioritizes patient safety and long-term mental health stability.
Funding and References
The study received no specific funding. Individuals with lived experiences contributed to the interpretation of results, ensuring the findings remain relevant to patient needs.
References
1. Zaccoletti D, Mosconi C, Gastaldon C, et al. Comparison of antidepressant deprescribing strategies in individuals with clinically remitted depression: a systematic review and network meta-analysis. Lancet Psychiatry. 2026;13(1):24-36. doi:10.1016/S2215-0366(25)00330-X. 2. Horowitz MA, Taylor D. Tapering of SSRI treatment to mitigate withdrawal symptoms. Lancet Psychiatry. 2019;6(6):538-546. 3. Guideline: NICE. Depression in adults: treatment and management. [NG222]. Published June 2022.