Highlights
In patients with localized radiorecurrent prostate cancer, salvage focal therapy (sFT) demonstrated a 10-year cancer-specific survival (CSS) of 92%, which was not statistically different from the 99% CSS observed in the salvage radical prostatectomy (sRP) cohort.
Overall survival (OS) at 10 years remained comparable between the two groups, suggesting that the less invasive nature of focal therapy does not compromise long-term oncological outcomes for appropriately selected patients.
The safety profile favored focal therapy significantly; patients undergoing sRP faced 24 times higher odds of experiencing any perioperative complication and 9 times higher odds of major complications (Clavien-Dindo Grade 3-5) compared to those receiving sFT.
This study provides the first long-term comparative evidence supporting sFT as a viable alternative to the traditional surgical gold standard, offering a more favorable therapeutic ratio.
Background: The Challenge of Radiorecurrent Prostate Cancer
Primary radiotherapy, including external beam radiation (EBRT) and brachytherapy, is a standard-of-care curative treatment for localized prostate cancer. However, biochemical recurrence occurs in approximately 20% to 50% of patients within ten years. For those whose recurrence is confined to the prostate, the clinical objective is to achieve local control while minimizing the severe morbidity often associated with salvage treatments.
Historically, salvage radical prostatectomy (sRP) has been considered the definitive local salvage option. However, sRP is technically demanding due to radiation-induced fibrosis, which obliterates surgical planes and increases the risk of rectal injury, urinary incontinence, and anastomotic leaks. Consequently, many patients and clinicians opt for androgen deprivation therapy (ADT), which is palliative rather than curative and carries its own burden of metabolic and cardiovascular side effects.
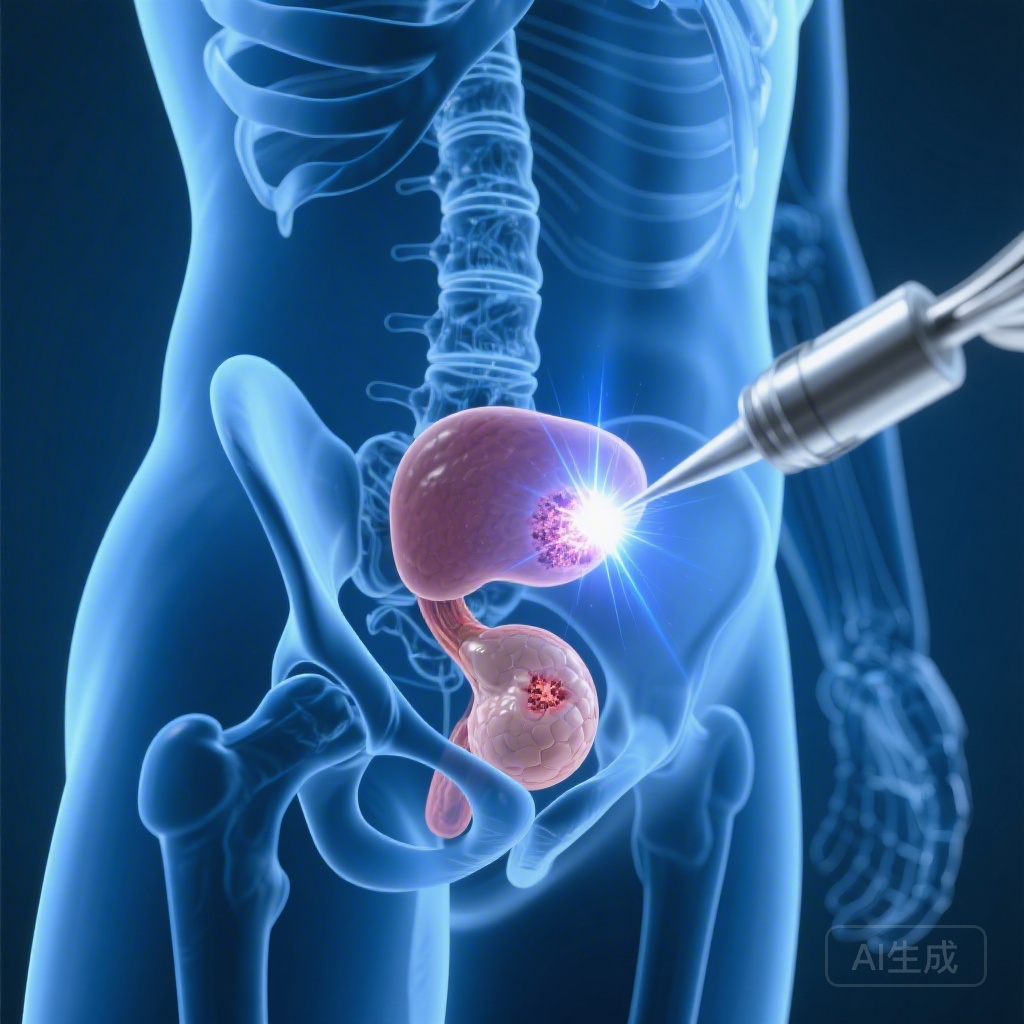
Salvage focal therapy (sFT), utilizing modalities such as high-intensity focused ultrasound (HIFU) or cryotherapy, has emerged as a middle-ground approach. By targeting only the site of recurrence within the gland, sFT aims to preserve surrounding structures like the neurovascular bundles and the urinary sphincter. Until now, the lack of long-term comparative data beyond five years has limited the widespread adoption of sFT in clinical guidelines.
Study Design and Methodology
This international, multicenter cohort study, published by Light et al. (2026) in JAMA Oncology, sought to address this evidence gap by comparing the oncological and safety outcomes of sFT versus sRP over a 10-year horizon.
Patient Population and Matching Process
The researchers utilized data from several prospective and retrospective registries across the UK, Europe, and the US. The sFT cohort (n=419) was derived from the UK HIFU Evaluation and Treatment, International Cryotherapy Evaluation, and the UK FORECAST study. The sRP cohort (n=504) came from an international retrospective registry spanning 12 centers in 8 countries. All patients had biopsy-confirmed, localized recurrence following primary radiotherapy.
To ensure a fair comparison, the study employed 1:1 cardinality matching within multiply-imputed datasets. The matching criteria were rigorous, accounting for the type of primary radiotherapy, the interval between primary and salvage treatment, EAU recurrence risk groups, pre-salvage PSA levels, prostate volume, Gleason grade group, T stage, and the use of ADT.
Interventions: sFT and sRP
Within the sFT group, 77.6% of patients underwent HIFU, while the remainder received cryotherapy. Over half of the sFT patients (57.5%) were treated with quadrant ablation. In the sRP group, 74.6% underwent traditional open surgery, with the rest receiving robot-assisted radical prostatectomy (RARP). This distribution reflects the evolving surgical landscape over the study period (2000-2024).
Key Findings: Survival and Cancer Control
The primary endpoint was cancer-specific survival (CSS) at 10 years, a critical measure for determining if focal therapy can match the curative potential of radical surgery.
Cancer-Specific and Overall Survival
The analysis revealed that sFT and sRP provided remarkably similar long-term oncological protection. The 10-year CSS was 92% (95% CI, 86%-98%) for sFT compared to 99% (95% CI, 97%-100%) for sRP. While the point estimate for sRP was higher, the difference was not statistically significant (P = 0.15). The subdistribution hazard ratio was 0.45 (95% CI, 0.05-4.00; P = 0.47), further confirming that the risk of prostate cancer death did not differ significantly between the two modalities.
Similarly, there was no statistically significant difference in 10-year overall survival (OS). The restricted mean survival time difference was a negligible -0.13 years (P = 0.72). These findings suggest that for patients with localized recurrence, the choice of salvage modality does not fundamentally alter their decade-long survival trajectory.
Perioperative Safety and Complications
The most striking differences emerged in the safety profiles. Salvage surgery post-radiation is notorious for its high complication rates, and this study quantified that risk in comparison to focal therapy. Patients undergoing sRP were significantly more likely to experience any perioperative complication (adjusted OR, 24.20; 95% CI, 12.94-45.27; P < 0.001).
More importantly, the risk of major complications (Clavien-Dindo grades 3 to 5), which require surgical, endoscopic, or radiological intervention, was nearly ten times higher in the sRP group (adjusted OR, 9.31; 95% CI, 3.42-25.36; P < 0.001). This confirms that while sRP is an oncologically robust procedure, it carries a substantial burden of morbidity that sFT largely avoids by minimizing collateral tissue damage.
Clinical Implications and Expert Commentary
The results of this study represent a significant shift in the salvage landscape. The high CSS in the sRP group (99%) reinforces its status as a highly effective oncological intervention. However, the 92% CSS in the sFT group, combined with its markedly lower complication rate, suggests that sFT offers a superior “therapeutic ratio” for many patients.
The Therapeutic Ratio
In clinical medicine, the therapeutic ratio is the balance between the desired effect (cancer control) and the adverse effects (complications). For a patient facing the prospect of salvage treatment, the trade-off between a 7% difference in 10-year CSS (which did not reach statistical significance) and a nearly 25-fold increase in complication risk is a critical decision point. For many, the preservation of quality of life—specifically urinary and sexual function, which are often severely impacted by sRP—will make sFT the preferred choice.
Study Limitations
Despite the strengths of the study, including the large multicenter cohorts and the 10-year follow-up, certain limitations must be acknowledged. This was a non-randomized study. Although cardinality matching was used to minimize selection bias, unmeasured confounders (such as surgeon experience or specific patient comorbidities) could still influence the results. Furthermore, the sRP cohort was predominantly composed of open surgical cases, which may have higher complication rates than modern robot-assisted series, although the risk of radiation-damaged tissue remains high regardless of the surgical platform.
Conclusion
The study by Light et al. provides much-needed evidence that salvage focal therapy is an effective and safer alternative to radical prostatectomy for localized radiorecurrent prostate cancer. With 10-year cancer-specific survival rates that are statistically comparable and a complication profile that is significantly more favorable, sFT should no longer be viewed as an experimental option. It should be discussed as a standard-of-care salvage strategy, particularly for patients who prioritize the preservation of functional outcomes and the avoidance of major surgical morbidity.
References
1. Light A, Peters M, Arya M, et al. Salvage Focal Therapy vs Radical Prostatectomy for Localized Radiorecurrent Prostate Cancer. JAMA Oncol. 2026;12(2):e256448. doi:10.1001/jamaoncol.2025.6448.
2. Chade DC, Shariat SF, Cronin AM, et al. Salvage radical prostatectomy for radiation-recurrent prostate cancer: a multi-institutional collaboration. Eur Urol. 2011;60(2):265-273.
3. Valle LF, Lehrer EJ, Deasy JO, et al. A Systematic Review and Meta-analysis of Local Salvage Therapies After Radiotherapy for Prostate Cancer (MASTER). Eur Urol. 2021;80(3):280-292.