Highlights
- A multicenter study of 408 patients found no significant difference in structural or biochemical incomplete responses between patients receiving total thyroidectomy alone versus those receiving adjuvant radioactive iodine (RAI) therapy.
- The lymph node metastasis ratio (LNR) was identified as a powerful independent predictor of structural recurrence, with a hazard ratio of 5.130.
- Treatment parameters such as RAI dosage, frequency, and postoperative interval did not significantly influence the risk of incomplete treatment response in T1-T2 stage papillary thyroid carcinoma.
Clinical Context and the RAI Debate
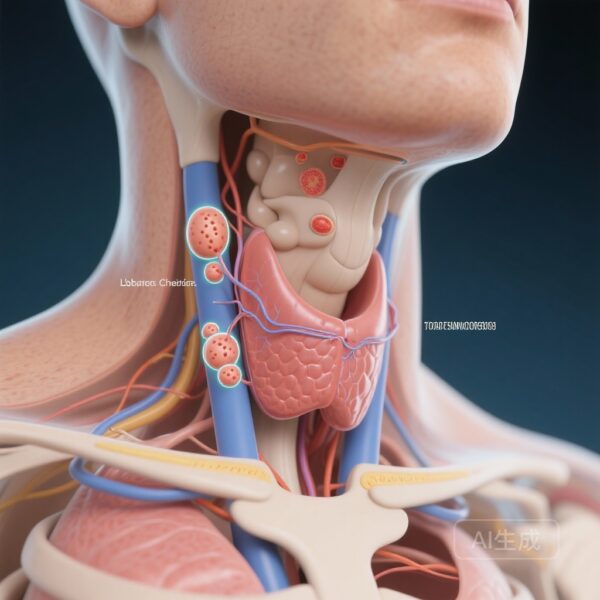
For decades, radioactive iodine (RAI) therapy has been a cornerstone of postoperative management for differentiated thyroid carcinoma (DTC). Its primary goals are the ablation of remnant thyroid tissue, adjuvant treatment of suspected micrometastasis, and therapy for known persistent disease. However, the clinical utility of RAI in low-to-intermediate risk patients—specifically those with T1-T2 stage papillary thyroid carcinoma (PTC) and cervical lymph node metastasis—remains a subject of intense debate within the endocrinology and oncology communities.
Current guidelines, including those from the American Thyroid Association (ATA), have moved toward a more selective approach to RAI, yet clinical practice varies significantly across global regions. In China, where the incidence of PTC has risen sharply, clinicians often face the challenge of balancing the potential benefits of RAI against its side effects, such as sialadenitis, xerostomia, and the risk of secondary malignancies. This multicenter analysis aims to clarify whether RAI therapy truly provides a survival or recurrence benefit for this specific patient population.
Study Design and Methodology
This research utilized a robust multicenter framework, drawing data from major thyroid cancer centers across China. The cohort included 408 patients diagnosed with T1-T2 stage PTC and pathologically confirmed cervical lymph node metastasis who underwent total thyroidectomy (TT). The data collection, spanning from 2015 to 2022, was prospectively standardized to ensure high-quality clinical and pathological parameters.
To address the inherent selection bias in retrospective observational data, the researchers employed Propensity Score Matching (PSM). This statistical technique balanced baseline characteristics between the group that received TT plus RAI (n=280) and the group that underwent TT alone. The primary endpoints were Structural Incomplete Response (SIR), characterized by persistent or recurrent disease on imaging, and Biochemical Incomplete Response (BIR), defined by elevated thyroglobulin levels in the absence of localizable disease. Multivariate Cox regression and Kaplan-Meier survival analysis were used to identify risk factors and compare recurrence-free survival (RFS) across the groups.
Key Research Findings
Recurrence and Response Rates
During a median follow-up period of 76.8 months, the overall rate of incomplete response was 10.0%, with 18 patients experiencing SIR and 23 experiencing BIR. These figures underscore that even in early-stage (T1-T2) PTC with nodal involvement, a small but significant portion of patients will face persistent or recurrent disease, necessitating a clear understanding of therapeutic efficacy.
Impact of Radioactive Iodine Therapy
The core finding of the study was that RAI therapy did not significantly alter the primary outcomes. After PSM, the rates of SIR and BIR remained statistically comparable between the TT+RAI cohort and the TT-only group (P > 0.05). Furthermore, Kaplan-Meier analysis revealed no significant difference in structural or biochemical recurrence-free survival. These results suggest that for T1-T2 stage patients, the addition of RAI may not provide the protective effect traditionally assumed by many practitioners.
Predictors of Structural Incomplete Response
While RAI therapy itself was not a significant factor, the study identified the lymph node metastasis ratio (LNR)—the number of metastatic nodes divided by the total number of nodes excised—as a critical independent predictor of SIR. With a hazard ratio (HR) of 5.130 (95% CI: 1.194-22.051; P = 0.028), a higher LNR was strongly associated with a greater risk of structural recurrence. Interestingly, other factors such as the frequency of RAI sessions, the cumulative dosage administered, and the interval between surgery and RAI therapy were not found to be risk factors for SIR or BIR.
Clinical Interpretation and Expert Commentary
The Significance of the Lymph Node Metastasis Ratio
The identification of LNR as a potent predictor is highly relevant for clinical decision-making. In many surgical settings, the absolute number of positive lymph nodes is used to determine risk; however, LNR may provide a more nuanced reflection of the metastatic burden and the thoroughness of the surgical clearance. Clinicians should perhaps place more weight on LNR when assessing the need for aggressive follow-up or adjuvant interventions, rather than relying solely on T-stage or the presence of nodal metastasis alone.
De-escalation of Therapy in Low-to-Intermediate Risk PTC
This study aligns with a broader global trend toward the de-escalation of treatment for low-risk thyroid cancer. If RAI does not significantly reduce recurrence in T1-T2 patients with nodal involvement, many patients may be safely managed with total thyroidectomy and active surveillance. This could significantly reduce healthcare costs and spare patients from the potential morbidity associated with radioactive iodine exposure. However, it is essential to note that this study focused on T1-T2 stages; patients with T3-T4 disease or extensive extrathyroidal extension may still derive substantial benefit from RAI.
Conclusion
In conclusion, this multicenter analysis suggests that for patients with T1-T2 stage papillary thyroid carcinoma and cervical lymph node metastasis, the routine application of radioactive iodine therapy following total thyroidectomy does not appear to significantly improve structural or biochemical response rates. Instead, the lymph node metastasis ratio emerges as a far more reliable indicator of recurrence risk. These findings advocate for a more individualized approach to thyroid cancer management, where RAI is reserved for patients with higher risk profiles, while others may be spared unnecessary treatment without compromising long-term outcomes.
References
1. Li X, Wu Q, Zhao J, et al. Multicenter analysis of radioactive iodine therapy outcomes after total thyroidectomy for T1-T2 stage papillary thyroid carcinoma with cervical lymph node metastasis in China. Int J Surg. 2025;111(10):6931-6941. doi:10.1097/JS9.0000000000002838.
2. Haugen BR, Alexander EK, Bible KC, et al. 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid. 2016;26(1):1-133.
3. Schlumberger M, Leboulleux S. Current practice in patients with differentiated thyroid cancer. Nat Rev Endocrinol. 2021;17(3):176-188.