Highlights of the COMPARE-TAVI 1 Substudy
Among the key takeaways from the analysis of the COMPARE-TAVI 1 trial are the following:
1. A distinct phenotype of severe aortic stenosis (AS) exists, characterized by a normal stroke volume index (SVi ≥35 mL/m2) despite a reduced left ventricular ejection fraction (LVEF <50%), occurring in approximately 10.7% of patients undergoing transcatheter aortic valve implantation (TAVI).
2. This Normal-Flow, Low-Ejection Fraction (NF-LEF) phenotype is driven by eccentric left ventricular remodeling and a higher prevalence of concomitant moderate-to-severe aortic regurgitation, which helps maintain stroke volume despite impaired contractility.
3. NF-LEF patients possess more favorable diastolic properties and lower filling pressures compared to their Low-Flow, Low-Ejection Fraction (LF-LEF) counterparts.
4. Following TAVI, NF-LEF patients show significant functional and clinical improvements, with survival and time-to-event outcomes that do not differ significantly from those with normal flow and normal ejection fraction (NF-NEF).
Introduction: The Evolution of Aortic Stenosis Phenotyping
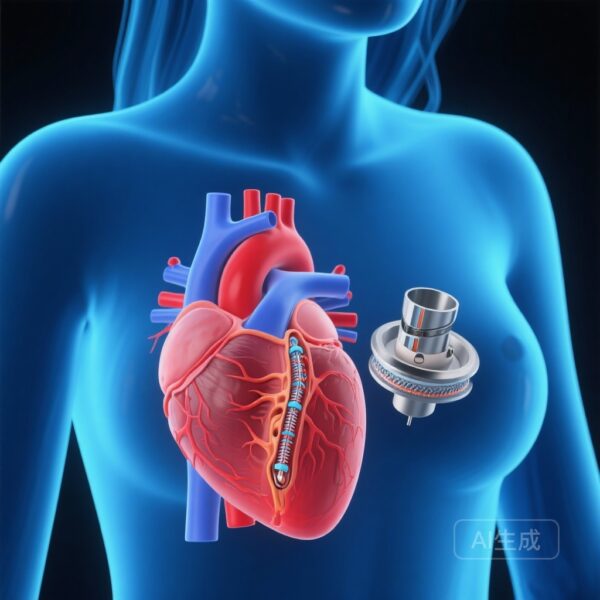
The clinical management of severe aortic stenosis has traditionally relied on the triad of valve area, mean gradient, and flow. However, the emergence of discordant grading—where valve area suggests severity but gradients remain low—has necessitated a more nuanced understanding of left ventricular (LV) remodeling and hemodynamics. While the low-flow, low-gradient (LF-LG) phenotype is well-documented in clinical guidelines, the paradoxical existence of normal flow in the setting of a reduced ejection fraction (NF-LEF) has remained relatively under-explored.
In classical hemodynamics, a reduction in LVEF is expected to correlate with a decrease in stroke volume. However, the NF-LEF phenotype challenges this assumption. It represents a state where the heart compensates for reduced contractile function through chamber dilation (eccentric hypertrophy), thereby maintaining a normal stroke volume index. Understanding this cohort is critical for clinicians, as these patients may present with misleadingly low gradients that mask the true severity of their valvular obstruction. The COMPARE-TAVI 1 substudy provides essential insights into the prevalence, morphological characteristics, and clinical trajectory of these patients following TAVI.
Study Design and Methodology
The COMPARE-TAVI 1 trial was a randomized controlled study involving patients undergoing transfemoral TAVI. This specific substudy analyzed 979 patients, stratifying them into four distinct hemodynamic groups based on baseline LVEF (cutoff of 50%) and SVi (cutoff of 35 mL/m2):
1. Normal Flow, Normal Ejection Fraction (NF-NEF): SVi ≥35 mL/m2, LVEF ≥50%
2. Normal Flow, Low Ejection Fraction (NF-LEF): SVi ≥35 mL/m2, LVEF <50%
3. Low Flow, Normal Ejection Fraction (LF-NEF): SVi <35 mL/m2, LVEF ≥50%
4. Low Flow, Low Ejection Fraction (LF-LEF): SVi <35 mL/m2, LVEF <50%
The primary objectives were to assess the prevalence of the NF-LEF phenotype, characterize its underlying ventricular morphology and diastolic function, and evaluate long-term outcomes, including survival, NYHA functional class improvement, and 6-minute walk distance (6MWD) at one year post-procedure.
Results: Characterizing the NF-LEF Phenotype
Morphological and Hemodynamic Distinctness
The NF-LEF phenotype was identified in 10.7% of the total cohort. These patients were clinically complex, often presenting with a history of myocardial infarction, permanent pacemakers, and higher baseline NYHA classes. Interestingly, NF-LEF patients exhibited significantly larger left ventricular end-diastolic and end-systolic volumes compared to all other groups. This eccentric remodeling allows the ventricle to eject a normal stroke volume despite a lower percentage of blood being pumped out with each beat.
A key driver of this phenotype appears to be the presence of concomitant aortic regurgitation (AR). Patients in the NF-LEF group were more likely to have moderate or worse AR (P=0.007) compared to those in the LF-LEF group. This regurgitant volume contributes to total stroke volume, explaining how flow is preserved even when the forward ejection fraction is diminished. Furthermore, NF-LEF patients demonstrated better diastolic indices, suggesting lower LV filling pressures than the LF-LEF group, which is typically characterized by restrictive filling patterns and concentric remodeling.
Clinical and Functional Outcomes
One of the most significant findings of the study was the post-TAVI recovery profile. Both the NF-LEF and LF-LEF groups showed significant improvements in LVEF following the relief of pressure overload. Specifically, SVi increased significantly in both low-flow groups (P<0.001).
Functional improvement was robust across all phenotypes. At the one-year mark, patients with NF-LEF showed improvements in 6MWD and NYHA class that were comparable to the NF-NEF group. In contrast, the LF-NEF group (often termed paradoxical low-flow, low-gradient AS) remained the most symptomatic and showed the least improvement in 6MWD, highlighting the particularly restrictive nature of that phenotype. Crucially, long-term survival and time-to-event outcomes did not differ significantly between the NF-LEF phenotype and the other groups, suggesting that TAVI is highly effective for these patients despite their higher baseline comorbidity burden.
Expert Commentary: Mechanistic Insights and Clinical Implications
The identification of the NF-LEF phenotype serves as a reminder that LVEF is a measure of contractility relative to chamber size, not a direct measure of absolute flow. In the setting of severe AS, the heart’s adaptation can take two divergent paths when contractility fails. The first is the well-known LF-LEF path, where the heart remains small or moderately hypertrophied but cannot maintain output. The second is the NF-LEF path, where the heart dilates.
From a clinical perspective, this study emphasizes that a normal stroke volume index should not lead clinicians to underestimate the impact of a reduced LVEF. These patients are often sicker, with more atrial fibrillation and mitral regurgitation, yet they possess a “functional reserve” in the form of chamber volume that allows them to maintain systemic perfusion. The fact that their survival post-TAVI matches that of patients with normal LVEF is encouraging and supports aggressive intervention in this subgroup.
However, the study also highlights the challenges of the LF-NEF group. These patients, often older women with small, stiff ventricles and concentric hypertrophy, represent a high-risk cohort that may not experience the same degree of functional rebound as those with larger, more compliant ventricles. This underscores the need for personalized hemodynamic assessment beyond simple valve area measurements.
Conclusion
The NF-LEF phenotype is a prevalent and clinically important subset of the aortic stenosis population. Characterized by eccentric remodeling and maintained flow, these patients represent a transition state where the heart compensates for reduced contractility through structural dilation. The COMPARE-TAVI 1 substudy demonstrates that NF-LEF patients benefit significantly from TAVI, achieving clinical and functional outcomes on par with patients who have preserved LVEF. Clinicians should remain vigilant in identifying this phenotype, ensuring that the presence of normal flow does not delay life-saving valvular intervention in the setting of reduced ventricular function.
References
1. Ravn EJ, et al. Paradoxical Normal-Flow Aortic Stenosis Despite Reduced Left Ventricular Ejection Fraction: Insights From the Randomized COMPARE-TAVI 1 Trial. J Am Heart Assoc. 2026;15(1):e045521.
2. Baumgartner H, et al. 2020 ESC/EACTS Guidelines for the management of valvular heart disease. Eur Heart J. 2021;42(6):561-653.
3. Clavel MA, et al. The Low-Flow, Low-Gradient Aortic Stenosis Phenotypes: Realities and Ambiguities. J Am Coll Cardiol. 2016;67(15):1813-1829.
4. Otto CM, et al. 2020 ACC/AHA Guideline for the Management of Patients With Valvular Heart Disease. Circulation. 2021;143(5):e35-e71.