Introduction: Expanding the Boundaries of Chronic Traumatic Encephalopathy
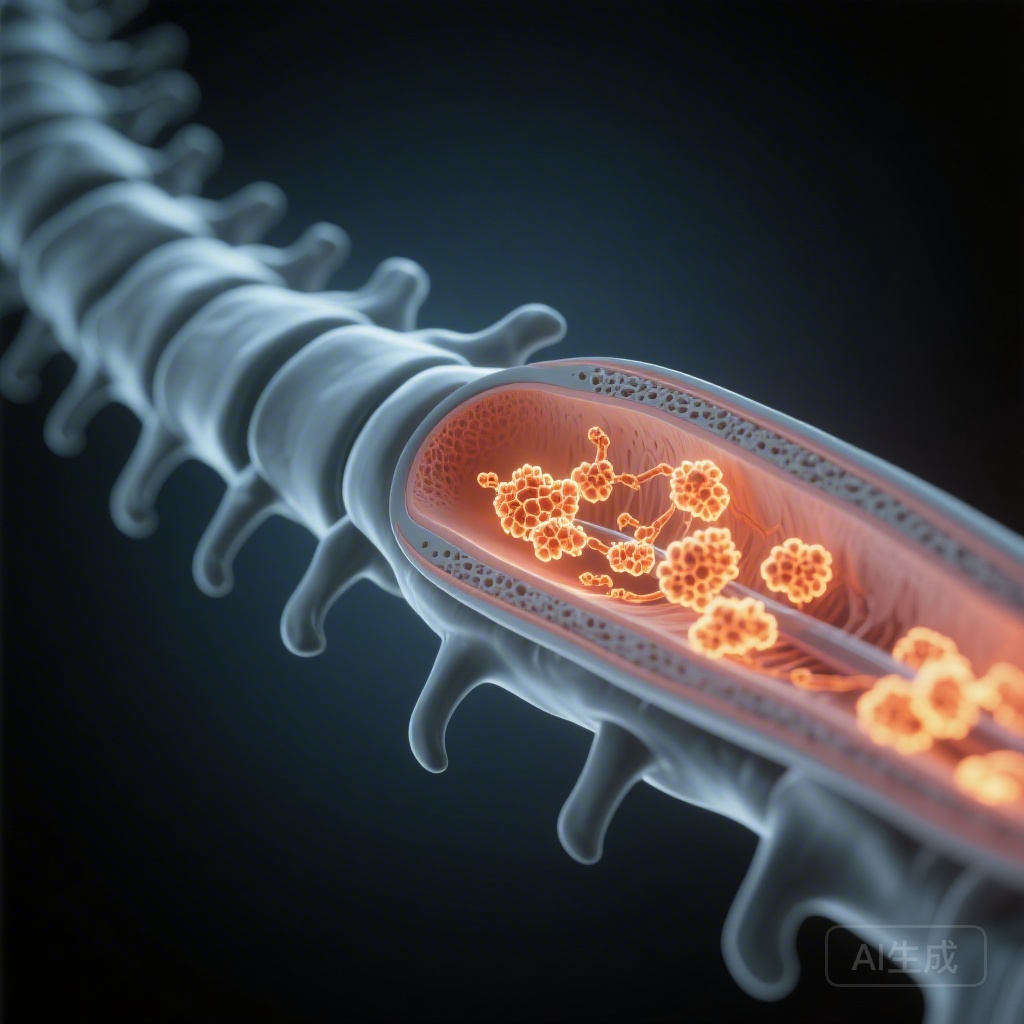
The medical understanding of Chronic Traumatic Encephalopathy (CTE) has traditionally focused on the cerebral cortex, specifically the pathognomonic accumulation of hyperphosphorylated tau (p-tau) in neurons and astrocytes around small blood vessels at the depths of the cortical sulci. However, emerging clinical evidence suggests that individuals exposed to repetitive head impacts (RHI) often present with a constellation of symptoms that extend beyond cognitive and behavioral changes, frequently involving motor dysfunction reminiscent of amyotrophic lateral sclerosis (ALS) or parkinsonism. A groundbreaking study by Tanaka et al., published in JAMA Neurology (2026), provides critical evidence that the pathology of CTE is not confined to the brain but represents a systemic trauma-related encephalomyelopathy involving the spinal cord.
The Clinical Imperative
Exposure to RHI, common in contact sports and military service, is a known risk factor for various neurodegenerative diseases. While the cortical manifestations of CTE neuropathologic change (CTE-NC) are well-documented, the involvement of the spinal cord has remained a significant gap in our understanding of the disease’s natural history. This study addresses whether the spinal cord is a primary site of protein misfolding following trauma and how these pathologies correlate with clinical motor symptoms.
Study Design and Methodology
This retrospective case-control study utilized an autopsy series from a multicenter brain bank collaboration, spanning from June 2019 to August 2025. The researchers analyzed the spinal cords of 70 individuals (62 male, 8 female; mean age 64.4 years).
Cohort Categorization
The participants were divided based on their history of RHI and the presence of CTE-NC in the brain:
The researchers employed advanced immunohistochemistry techniques to detect several key proteins: phosphorylated tau (p-tau), phosphorylated TAR DNA-binding protein 43 (p-TDP-43), α-synuclein, and amyloid-β (Aβ). Additionally, markers for neuroinflammation (HLA-DR) and axonal injury (amyloid precursor protein) were evaluated.
Key Findings: The Prevalence of Spinal Tauopathy
The most striking result of the study was the universal presence of spinal cord pathology in individuals with brain CTE-NC.
Universal Tau Involvement
Every single case (100%) that exhibited CTE-NC in the brain also showed p-tau deposits in the spinal cord. In contrast, while some individuals without CTE-NC (54%) showed sparse spinal p-tau, the severity and distribution were significantly lower. For those aged 65 or older with a history of RHI and CTE-NC, the pathology was particularly extensive, involving both neuronal and astrocytic p-tau deposits in the gray and white matter.
Complex Protein Copathologies
The study revealed that in older individuals (≥65 years), the spinal cord becomes a reservoir for multiple misfolded proteins. Among the 14 cases in this age bracket with CTE-NC:
Notably, in 50% of the cases where p-TDP-43 was present in the spinal cord, it was entirely absent from the brain, suggesting that the spinal cord may be uniquely susceptible to certain trauma-induced protein misfolding pathways.
Clinical Correlation and Neuroinflammation
The presence of these protein aggregates was not merely a pathological curiosity; it correlated with clinical manifestations and biological markers of distress.
Motor Symptoms and Microglial Activation
Spinal p-tau pathology was significantly associated with informant-reported motor symptoms, including weakness, gait instability, and tremors. Pathologically, these areas of protein accumulation were marked by intense microglial activation (HLA-DR positivity), indicating a chronic inflammatory state within the spinal cord.
The RHI Group Without CTE-NC
Interestingly, 70% of individuals with a history of RHI exhibited CTE-NC, while 30% did not. However, even in the group without formal CTE-NC, astrocytic tau pathology was observed in the spinal cord—a finding distinctly absent in the control group without RHI exposure. This suggests that spinal cord changes may precede or occur independently of the classic cortical stages of CTE.
Expert Commentary: Mechanistic Insights
The findings by Tanaka et al. suggest that the mechanical forces of RHI—likely involving rotational acceleration and axonal shearing—trigger a cascade of protein misfolding that propagates throughout the central nervous system.
The Concept of Encephalomyelopathy
The term “encephalomyelopathy” better captures the systemic nature of the damage. The spinal cord, with its long axonal tracts, may be particularly vulnerable to the tensile stresses of trauma. The co-occurrence of Aβ and α-synuclein suggests that RHI might impair the general proteostatic mechanisms of the spinal cord, leading to a “fertile ground” for various neurodegenerative processes to take root.
Study Limitations and Future Directions
While the study is robust, the retrospective nature and reliance on informant-reported symptoms are limitations. The cohort was also predominantly male, reflecting the demographics of contact sports, which may limit generalizability to female populations. Future research must determine whether spinal cord imaging or biomarkers (such as biofluid p-tau levels) can detect these changes in living patients.
Conclusion: Implications for Clinical Practice
This study provides definitive autopsy evidence that CTE is a multi-protein, multi-segmental disease. For clinicians, this highlights the importance of comprehensive neurological evaluations in RHI-exposed patients that look beyond cognitive decline to include subtle motor and spinal signs. The frequent presence of p-TDP-43 in the spine, even in the absence of brain pathology, underscores a potential link between RHI and motor neuron disease phenotypes. Ultimately, these findings advocate for a broader diagnostic framework and the development of therapies that can address the complex, multi-protein nature of trauma-related neurodegeneration.
References
1. Tanaka H, Black LE, Forrest SL, et al. Spinal Cord Tau and Protein Copathologies Associated With Chronic Traumatic Encephalopathy. JAMA Neurol. 2026; doi:10.1001/jamaneurol.2025.5421.
2. McKee AC, Stein TD, Kiernan PT, Alvarez VE. The Neuropathology of Chronic Traumatic Encephalopathy. Brain Pathol. 2015;25(3):350-364.
3. Stern RA, Daneshvar DH, Baugh CM, et al. Clinical presentation of chronic traumatic encephalopathy. Neurology. 2013;81(13):1122-1129.