Highlights
- Post-TAVR new-onset RBBB occurs in approximately 5.3 cases per 1,000 procedures.
- Nearly half of affected patients require a permanent pacemaker within one year, most within the first week after the procedure.
- Post-TAVR PR interval length ≥230 ms and PR change ≥24 ms help identify high-risk patients.
Background
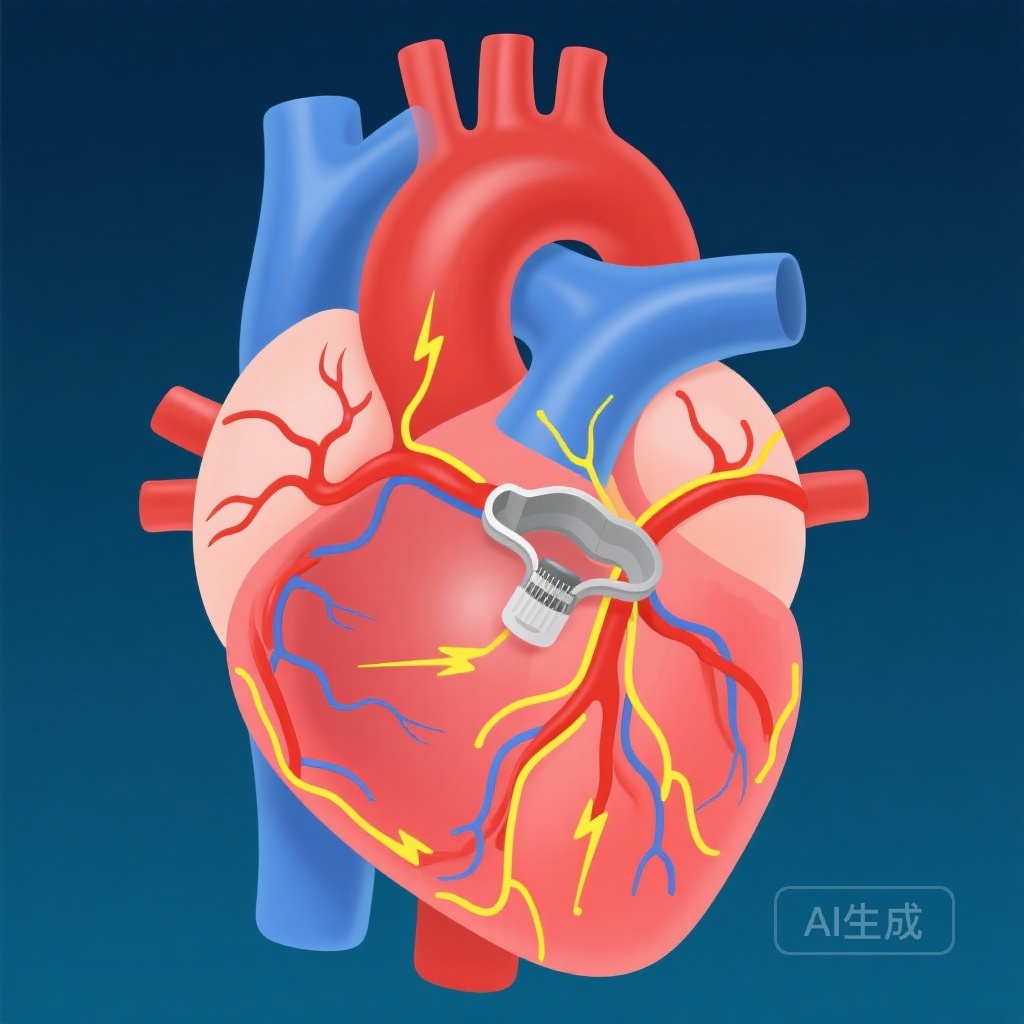
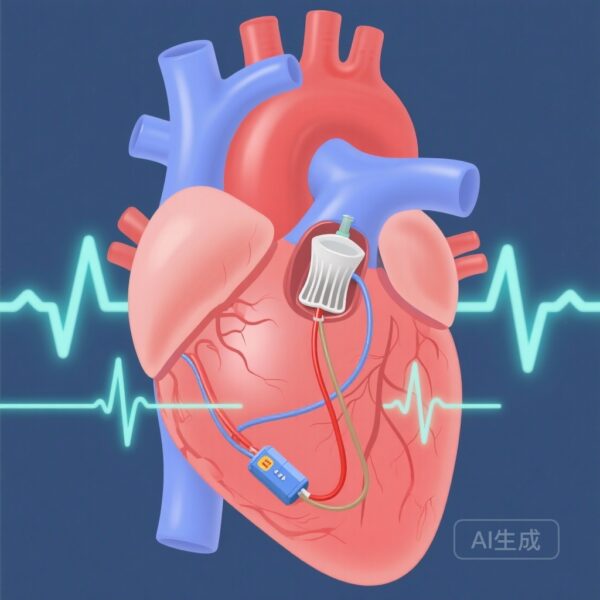
Transcatheter aortic valve replacement (TAVR) is a well-established treatment for severe aortic stenosis in patients across surgical risk profiles. Conduction disturbances following TAVR are common, particularly new-onset left bundle branch block (LBBB), often necessitating further cardiac rhythm management. In contrast, right bundle branch block (RBBB) post-TAVR has been considered uncommon and less studied. Given the anatomical proximity of the His-Purkinje system to the implanted valve, even rare disturbances may carry important implications for patient care.
Study Design
This multicenter retrospective cohort analysis was conducted across seven Israeli hospitals, evaluating 7,782 consecutive TAVR patients. All participants underwent baseline electrocardiograms within 48 hours prior to the procedure and daily follow-up ECGs thereafter. The study identified new-onset RBBB and monitored patients for one year, focusing on absolute pacing indications (API), defined as high-grade atrioventricular block or alternating bundle branch block. Permanent pacemaker implantation (PPI) rates, timing, and associations with PR interval changes were analyzed.
Key Findings
Among the cohort, 41 cases of post-TAVR new-onset RBBB were identified, corresponding to an incidence of 5.3 per 1,000 procedures (95% CI: 3.8–7.1). Within one year, 46.3% (19 patients) required PPI. Most PPIs were performed during the index hospitalization, with all but one API occurring before discharge. Late API was documented in just one patient due to delayed AV block. Analysis of electrophysiological markers revealed that a post-TAVR PR interval cutoff of 228 ms provided a specificity of 95% and sensitivity of 50% in predicting API. Similarly, a PR change (Δ PR) of ≥24 ms yielded 80% specificity and 83% sensitivity. Importantly, survival outcomes suggested a nonsignificant advantage for patients not undergoing PPI, although this finding warrants further study.
Timing of Conduction Deterioration
The majority of conduction system deterioration occurred within the first week after TAVR, underscoring the critical early post-procedure window for monitoring and intervention.
Risk Stratification Utility
Post-TAVR PR interval prolongation and Δ PR are practical markers for identifying patients at high risk for progressive conduction disease. PR ≥230 ms or Δ PR ≥24 ms should prompt heightened surveillance or consideration for early pacing decisions, especially in centers with high patient volumes and rapid discharge protocols.
Expert Commentary
The rarity of RBBB should not diminish its clinical significance post-TAVR. While LBBB remains the more frequent and studied conduction block, this research shows that RBBB carries a proportionally higher risk of progressing to conditions requiring pacing. From an anatomical standpoint, injury or mechanical compression of the right bundle branch can occur due to deployment depth and prosthesis geometry, particularly in self-expanding valves. Clinicians should integrate PR interval metrics into early postoperative monitoring workflows. However, PR interval thresholds, while useful, should not be the sole determinant; patient comorbidities, valve type, and procedural complexity also warrant consideration.
Limitations include the retrospective design and reliance on continuous ECG surveillance, which may not be feasible in all settings. Additionally, the study did not differentiate outcomes based on valve type, a factor known to influence conduction complication rates.
Conclusion
Post-TAVR new-onset RBBB, although rare, is strongly associated with progressive conduction abnormalities and a high likelihood of requiring permanent pacing, typically within one week post-procedure. PR interval assessment is a valuable, practical tool for risk stratification. Clinicians should remain vigilant in early post-TAVR monitoring, particularly for patients with significant PR prolongation. Prospective validation of suggested PR thresholds in diverse procedural contexts could further enhance predictive accuracy and patient outcomes.
Funding and ClinicalTrials.gov
No specific funding disclosures were noted. No registered clinical trial number provided.
References
Michowitz Y, Yagel O, Shrem M, Elbaz-Greener G, Tovia-Brodie O, Goldenberg GR, Danon A, Katz M, Taieb P, Loewenstein I, Shamia D, Kezerle L, Dvir D, Glikson M, Belhassen B. New-Onset RBBB After Transcatheter Aortic Valve Replacement: Incidence and Risk Factors for Permanent Pacemaker Implantation. JACC Clin Electrophysiol. 2025 Nov;11(11):2458-2467. doi: 10.1016/j.jacep.2025.06.013. Epub 2025 Aug 6. PMID: 40767801.