Highlight
Baseline quantitative leakage index on ultra-widefield fluorescein angiography (UWF-FA) is a significant independent predictor of a 2-step or greater worsening on the Diabetic Retinopathy Severity Scale (DRSS) over a four-year period.
An absolute increase in the retinal leakage index of 1% or more at the one-year follow-up mark is associated with a more than two-fold increase in the risk of disease progression and vision-threatening complications.
Automated quantitative leakage assessment provides a continuous, objective severity scale that may enhance clinical risk stratification beyond traditional categorical ETDRS grading systems.
Background: The Evolution of Diabetic Retinopathy Monitoring
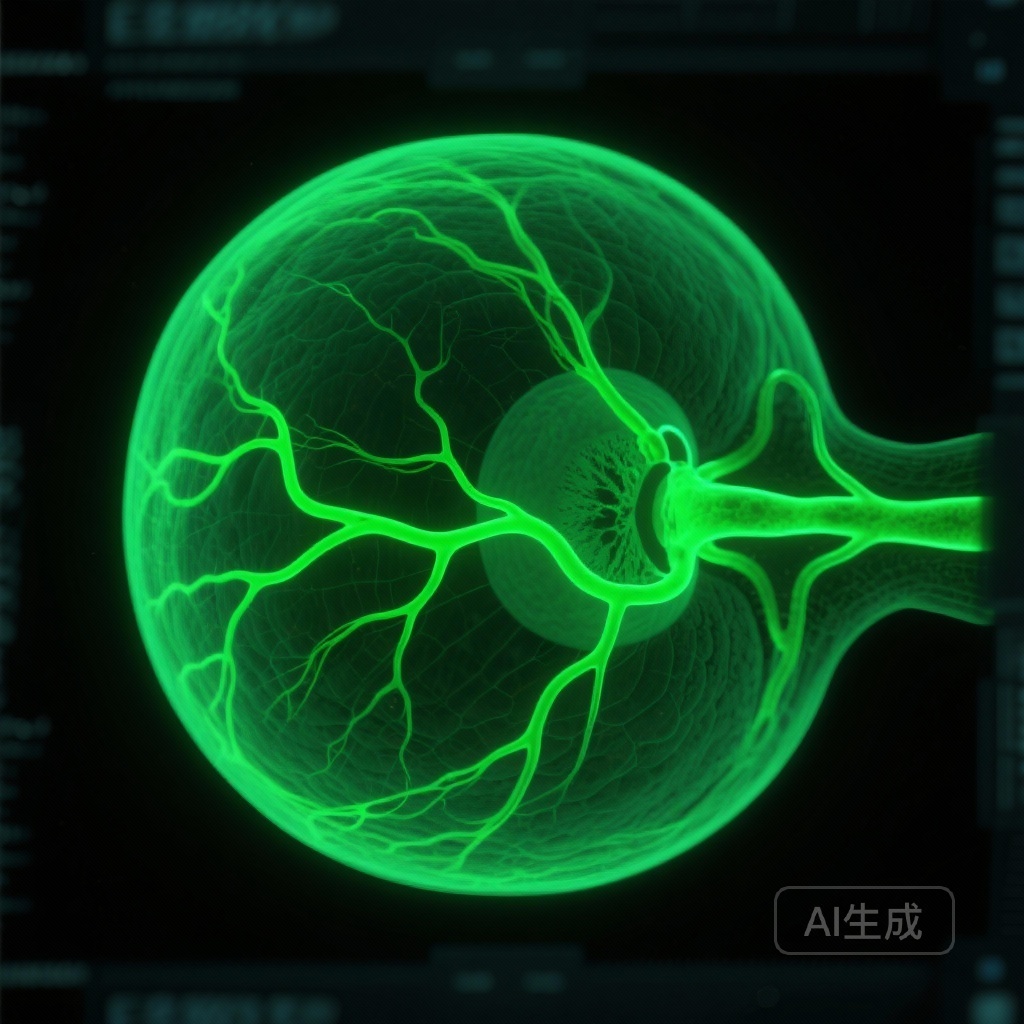
For decades, the management of diabetic retinopathy (DR) has relied heavily on the Early Treatment Diabetic Retinopathy Study (ETDRS) classification system. While the ETDRS Diabetic Retinopathy Severity Scale (DRSS) remains the gold standard for clinical trials and practice, it is fundamentally a categorical system based on structural features observed in color fundus photography. This approach, while robust, has inherent limitations: it is subjective, relies on a 30- to 50-degree field of view, and provides a ‘snapshot’ of structural damage rather than a dynamic measure of vascular physiology.
Fluorescein angiography (FA) has long been used to identify vascular pathology, but traditional FA also suffers from a limited field of view. The advent of ultra-widefield fluorescein angiography (UWF-FA) has revolutionized our ability to visualize the peripheral retina, where significant pathology often resides. However, until recently, the interpretation of UWF-FA remained largely qualitative. Clinicians would note the presence of ‘leakage’ or ‘nonperfusion,’ but lacked a standardized, reproducible method to quantify these features.
There is a critical unmet medical need for objective, continuous biomarkers that can predict which patients with nonproliferative diabetic retinopathy (NPDR) are at the highest risk for progression to proliferative diabetic retinopathy (PDR) or vitreous hemorrhage (VH). The recent study by Ehlers et al., published in JAMA Ophthalmology, addresses this gap by evaluating automated quantitative leakage parameters as prognostic indicators.
Study Design: The Protocol AA Post Hoc Analysis
This study represents a post hoc analysis of the Diabetic Retinopathy Clinical Research (DRCR) Retina Network Protocol AA. Protocol AA was a prospective, multicenter observational study designed to evaluate the utility of UWF imaging in patients with NPDR.
The analysis included 537 eyes from 363 adult participants with a mean age of 61 years. The participant pool was balanced by sex (50% male, 50% female). Data collection spanned from February 2015 to March 2020, with subsequent analysis performed between 2023 and 2024.
The primary intervention in the original trial was the observation of NPDR progression, with treatment for DR or diabetic macular edema (DME) administered at the investigator’s discretion. The researchers utilized a specialized automated software platform to calculate the ‘leakage index.’ This index is defined as the total area of fluorescein leakage divided by the total analyzable retinal area captured on UWF-FA.
Key endpoints evaluated over a 4-year follow-up period included:
1. Time to DRSS worsening of 2 or more steps.
2. Development of vitreous hemorrhage (VH).
3. Progression to proliferative diabetic retinopathy (PDR).
Key Findings: Baseline Leakage and the 4-Year Prognosis
The baseline mean leakage index across the cohort was 3.5% (SD, 3.9%). The researchers found a robust statistical association between this baseline measurement and the future risk of disease worsening.
Specifically, for every 1% increase in the baseline leakage index, there was a 9% increase in the risk of DRSS worsening over 4 years (Hazard Ratio [HR], 1.09; 95% CI, 1.05-1.13; P < .001). This suggests that even small variations in measurable vascular incompetence at the outset of observation carry significant prognostic weight.
Furthermore, baseline leakage was not only a predictor of gradual DRSS changes but also a harbinger of severe, vision-threatening events. Higher baseline leakage indices were significantly associated with the subsequent development of vitreous hemorrhage and the transition to full-blown proliferative disease.
The Impact of Longitudinal Change: The 1-Year Milestone
Perhaps the most clinically actionable finding from the study involves the change in leakage over time. The researchers evaluated the absolute change in the leakage index from baseline to the 1-year follow-up.
Among 453 eyes with available 1-year data, 25% (114 eyes) demonstrated an absolute increase in the leakage index of 1% or greater. The outcomes for this ‘progressor’ group were starkly different from those with stable leakage:
– Eyes with a >=1% increase in leakage had a 61% risk of DRSS worsening over 4 years.
– Eyes without such an increase had only a 33% risk.
– The adjusted Hazard Ratio for DRSS worsening in eyes with a >=1% leakage increase was 2.63 (95% CI, 1.90-3.64; P < .001).
This data indicates that longitudinal monitoring of quantitative leakage can identify a high-risk subset of patients who might benefit from more frequent monitoring or earlier therapeutic intervention, such as anti-VEGF therapy or closer metabolic control.
Expert Commentary: Moving Toward Precision Ophthalmology
The integration of automated quantitative assessments into clinical workflow represents a paradigm shift in the management of diabetic eye disease. By moving from a subjective ‘present vs. absent’ assessment of leakage to a continuous scale, clinicians can better appreciate the spectrum of disease activity.
From a mechanistic perspective, fluorescein leakage is a direct proxy for the breakdown of the blood-retinal barrier, driven primarily by vascular endothelial growth factor (VEGF) and inflammatory cytokines. While nonperfusion (ischemia) tells us about vascular ‘death,’ leakage tells us about vascular ‘dysfunction.’ The fact that leakage independently predicts progression suggests that physiologic stress on the vessels often precedes the structural changes traditionally captured by the DRSS.
However, some limitations must be considered. This was a post hoc analysis, and while the data is derived from a high-quality clinical trial (Protocol AA), the results require validation in prospective, independent cohorts. Additionally, the automated software used for quantification is not yet universally available in all clinical platforms, and standardization across different UWF imaging hardware (e.g., Optos vs. Heidelberg) remains a challenge.
Summary and Clinical Implications
The study by Ehlers and the DRCR Retina Network provides compelling evidence that UWF-FA quantitative leakage parameters are powerful biomarkers for NPDR progression. In an era where personalized medicine is becoming the standard of care, these findings offer a roadmap for more precise risk stratification.
Key takeaways for clinicians include:
1. Baseline leakage matters: Patients with higher levels of leakage on initial UWF-FA should be monitored more closely, regardless of their ETDRS grade.
2. Longitudinal change is a red flag: A 1% increase in the leakage index over a year is a potent predictor of imminent progression to PDR or VH.
3. Automation is the future: Quantitative metrics reduce inter-observer variability and provide a more nuanced view of retinal health than qualitative assessments alone.
As AI-driven image analysis continues to mature, it is likely that quantitative leakage indices will become a standard component of retinal imaging reports, helping to guide treatment decisions and improve long-term visual outcomes for patients with diabetes.
Funding and References
This research was supported by grants from the National Eye Institute and the National Institute of Diabetes and Digestive and Kidney Diseases, parts of the National Institutes of Health. The study was conducted by the DRCR Retina Network.
References:
1. Ehlers JP, Josic K, Aiello LP, et al. Ultra-Widefield Fluorescein Angiographic Quantitative Leakage Parameters and Clinical Outcomes in Nonproliferative Diabetic Retinopathy. JAMA Ophthalmol. 2026; doi:10.1001/jamaophthalmol.2025.5658.
2. Silva PS, Marcus DM, Quintana RP, et al.; DRCR Retina Network. Peripheral Lesions Identified on Ultra-widefield Imaging Predict Risk of Diabetic Retinopathy Worsening Over 4 Years. JAMA Ophthalmol. 2022;140(10):936-945.
3. Aiello LP, Odia I, Glassman AR, et al.; DRCR Retina Network. Comparison of Ultra-widefield Fluorescein Angiography With 7-Field Fundus Photographs for Tiered Diabetic Retinopathy Grading. JAMA Ophthalmol. 2019;137(1):65-73.