Background
Peripheral arterial disease (PAD) is characterized by progressive arterial narrowing, most commonly due to atherosclerosis, leading to reduced blood supply to the limbs. In severe cases, peripheral arterial reconstruction—via open or hybrid techniques—is required to restore perfusion and prevent limb loss. While these procedures can be life- and limb-saving, they carry a notable risk of graft infections and surgical site infections (SSIs), which can result in high morbidity, repeated interventions, and increased healthcare costs.
Preventing infection in vascular surgery, especially in groin incisions and graft implantation sites, is a critical element of perioperative care. Strategies vary from systemic antibiotic prophylaxis to advanced wound management technologies. A recent Cochrane systematic review synthesizes evidence from randomized and quasi-randomized controlled trials addressing pharmacological and non-pharmacological measures to minimize infection risk.
Study Design
This review included 35 randomized controlled trials (RCTs) and 5 quasi-RCTs, altogether involving 7,970 participants undergoing open or hybrid lower limb peripheral arterial reconstruction. Trials evaluated different interventions:
- Prophylactic antibiotics versus placebo or no treatment
- Short-duration (≤ 24 hours) versus prolonged (> 24 hours) antibiotic prophylaxis
- Comparisons between different systemic antibiotic regimens
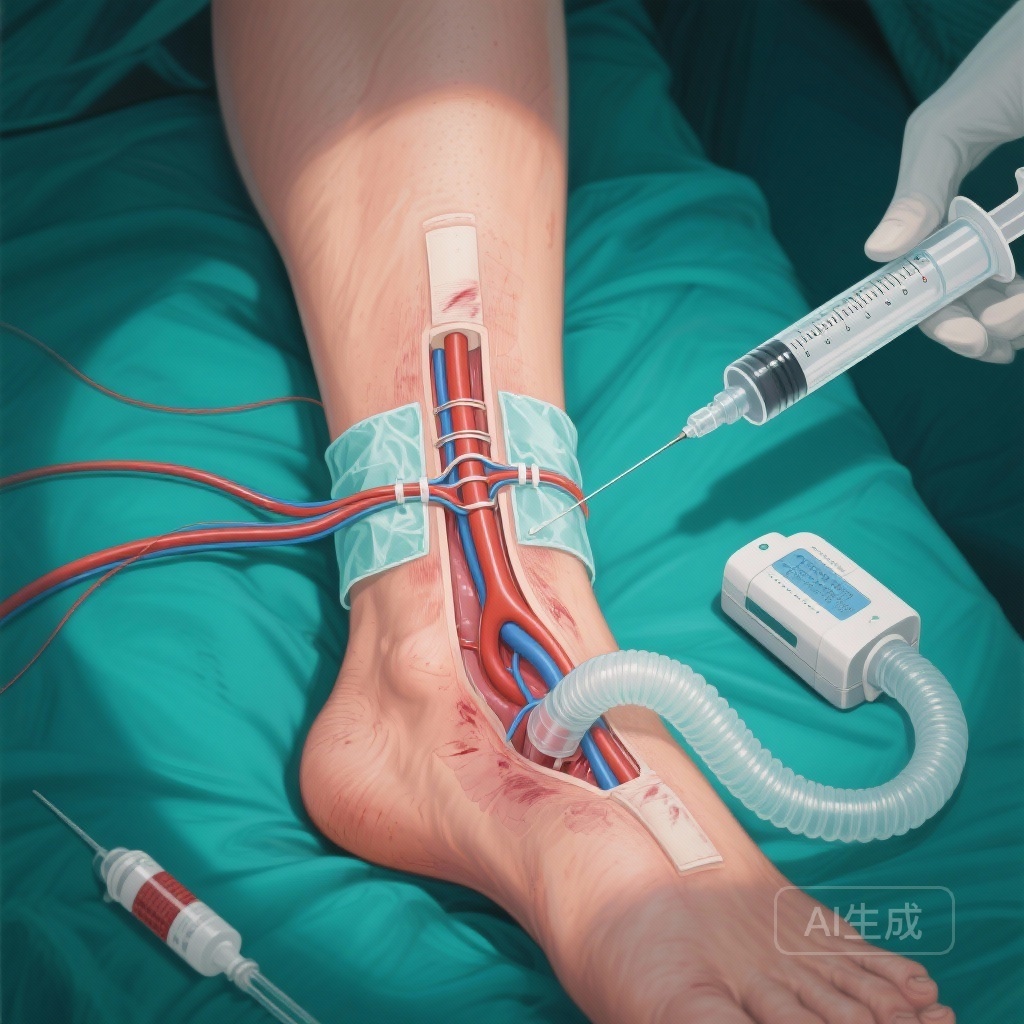
- Closed incision negative pressure therapy (NPWT) versus standard wound closure
Primary endpoints were graft infection rate and SSI rate. Secondary outcomes included all-cause mortality, reconstruction failure, re-intervention, amputation, pain, health-related quality of life, and adverse events.
Key Findings
1. Prophylactic antibiotics versus placebo
Across eight studies (1,188 participants for SSI outcomes), prophylactic antibiotics were associated with a markedly reduced SSI rate (Risk Ratio [RR] 0.20, 95% Confidence Interval [CI] 0.11–0.34; low-certainty evidence), with a number needed to treat (NNT) of 9. For graft infection rate, data from six studies suggested benefit (RR 0.19, 95% CI 0.06–0.63; NNT 5; low-certainty evidence). Differences in mortality, graft failure, and amputation were not statistically significant.
2. Short- versus long-duration antibiotic prophylaxis
Three studies indicated little or no significant difference between ≤ 24 hours and > 24 hours antibiotic prophylaxis for graft infection (RR 1.40, 95% CI 0.09–20.65) or SSI rate (RR 0.75, 95% CI 0.40–1.40). The certainty of evidence was very low, suggesting that prolonged regimens may not be clearly more effective than shorter ones.
3. Different systemic antibiotics
Seven trials compared one antibiotic regimen with another, including cephalosporin generations, fluoroquinolones, and glycopeptides. No statistically significant superiority emerged among antibiotic classes. For example, the SSI rate comparison between second-/third- generation cephalosporins and first-generation cephalosporins yielded RR 0.71 (95% CI 0.26–1.97; very low-certainty evidence).
4. Closed incision negative pressure therapy (NPWT)
Nine studies examined NPWT versus standard wound closure. A possible reduction in SSI rate was observed (RR 0.49, 95% CI 0.27–0.86; very low-certainty evidence), though differences in graft infection rates were not conclusive (RR 0.55, 95% CI 0.19–1.59). Secondary endpoints including mortality, re-intervention, and pain showed no significant differences.
Expert Commentary
These findings support the perioperative use of prophylactic antibiotics in lower limb peripheral arterial reconstruction, with the strongest—albeit low-certainty—evidence for reducing SSI and graft infection rates. Importantly, extension of prophylaxis beyond 24 hours appears unwarranted based on current data, which aligns with antimicrobial stewardship principles aimed at limiting resistance and adverse events.
The lack of clear superiority among antibiotic types suggests that regimen choice should align with local pathogen profiles and resistance patterns, rather than perceived class advantage. Closed incision NPWT shows potential for SSI reduction in high-risk groin wounds, but its routine use should be weighed against cost, resource availability, and inconclusive evidence strength.
Conclusion
Infection prevention remains a cornerstone of successful vascular surgery outcomes. Low-certainty evidence favors the use of perioperative prophylactic antibiotics, but prolonged courses or specific antibiotic switches have little demonstrable additional effect. Closed incision NPWT may confer benefit for SSI reduction, but further high-quality trials are needed. Clinicians should individualize infection prevention strategies based on patient risk factors, institutional protocols, and resource considerations.
Funding and ClinicalTrials.gov
This review was conducted under Cochrane Vascular guidelines. Registered searches included the WHO International Clinical Trials Registry Platform and ClinicalTrials.gov (up to August 26, 2024).
References
Correia RM, Nakano LC, Vasconcelos V, Cristino MA, Flumignan RL. Prevention of infection in peripheral arterial reconstruction of the lower limb. Cochrane Database Syst Rev. 2025 Oct 29;10(10):CD015022. doi: 10.1002/14651858.CD015022.pub2. PMID: 41159585; PMCID: PMC12570293.