Introduction and Context
For decades, ovarian cancer was thought to originate primarily within the ovaries themselves. However, a revolutionary shift in our understanding of gynecological oncology has identified the fallopian tube epithelium—specifically the distal end—as the primary site of origin for the majority of high-grade serous ovarian carcinomas (HGSOC). HGSOC is the most common and lethal form of the disease, often diagnosed at an advanced stage when prognosis is poor.
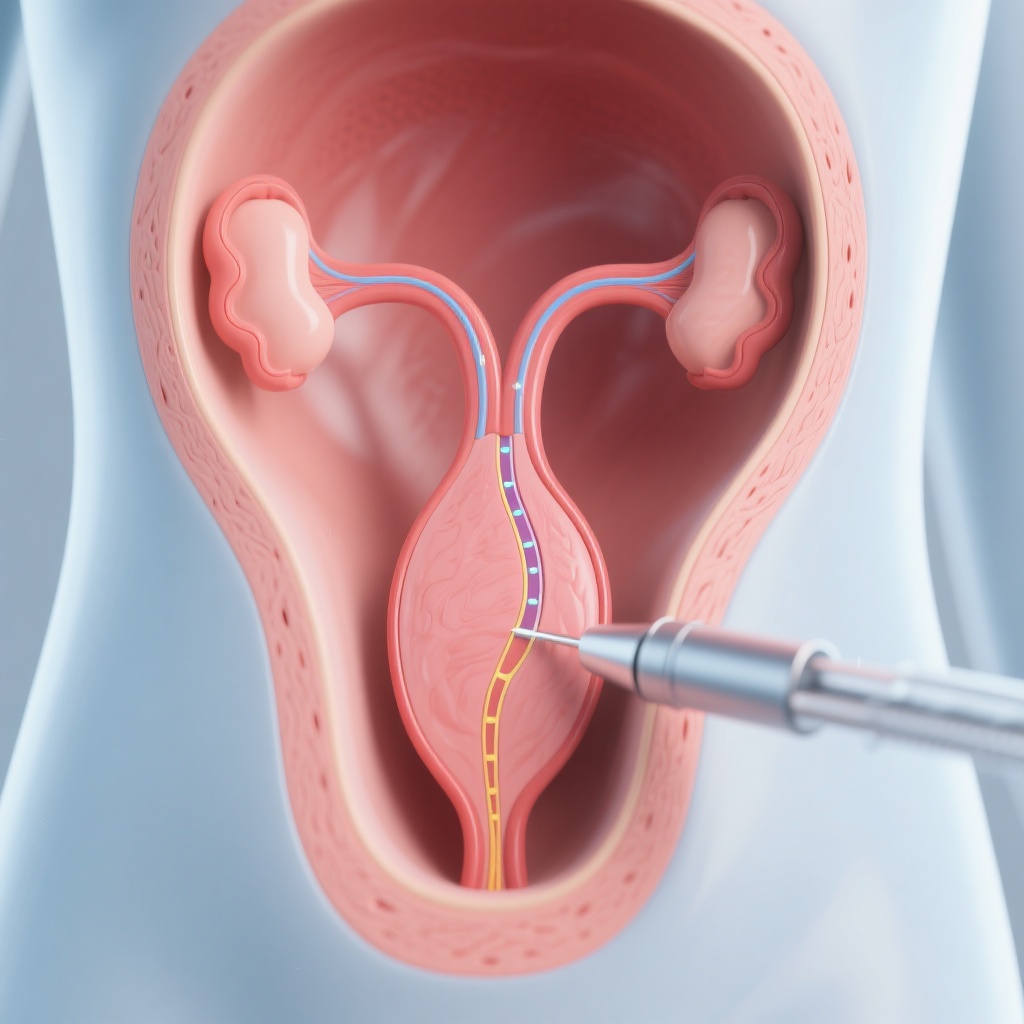
This paradigm shift has led to the concept of **opportunistic salpingectomy (OS)**: the removal of the fallopian tubes during a pelvic or abdominal surgery that is being performed for another reason (such as a hysterectomy, sterilization, or even non-gynecological procedures like gallbladder removal). By removing the tissue where the cancer starts, clinicians can theoretically prevent the disease before it ever reaches the ovaries. To standardize this practice, the European Society of Gynaecological Oncology (ESGO) recently convened an international working group to develop the 2026 Consensus Statements on Opportunistic Salpingectomy, providing a clear roadmap for clinicians worldwide.
New Guideline Highlights
The ESGO consensus represents a significant milestone in cancer prevention. The working group, which included 14 experts and a patient representative, performed an exhaustive review of literature from 2000 to 2025. Their findings underscore a critical takeaway: opportunistic salpingectomy is safe, effective, and should be a standard component of preoperative counseling for women undergoing abdominal or pelvic surgeries.
Key highlights include:
- Significant Risk Reduction: Removal of the fallopian tubes is strongly associated with a lower incidence of subsequent tubo-ovarian carcinoma.
- Preservation of Hormonal Health: Unlike oophorectomy (removal of ovaries), salpingectomy does not appear to negatively impact ovarian reserve or trigger premature menopause.
- Broad Feasibility: The procedure is feasible during both gynecological and selected non-gynecological surgeries.
- Clinical Counseling: Proactive discussion of OS is recommended for all eligible women regardless of their genetic risk profile.
Topic-by-Topic Recommendations
The ESGO consensus consists of 18 specific statements. These are categorized by clinical application, safety, and patient communication.
1. Efficacy in Cancer Prevention
The panel reached a high level of consensus that OS is a primary prevention strategy for HGSOC. While the gold standard—randomized controlled trials with long-term survival data—is still in progress, existing observational data and population-based studies provide compelling evidence of a protective effect. The consensus grades these recommendations from B to D, reflecting the strength of current epidemiological evidence.
2. Impact on Ovarian Function
A major concern for patients and clinicians is whether interfering with the blood supply to the ovaries during tube removal might lead to early menopause. The consensus states that current evidence (Level II to III) shows no adverse short-term impact on anti-Müllerian hormone (AMH) levels, which is a proxy for ovarian reserve. Patients can be reassured that their hormonal balance and timing of menopause are unlikely to be affected by the procedure.
3. Surgical Safety and Complexity
Adding a salpingectomy to another procedure typically adds only 10 to 15 minutes of operative time. The consensus confirms that OS does not significantly increase the risk of intraoperative or postoperative complications, such as blood loss, infection, or length of hospital stay. It is considered safe across various surgical approaches, including laparoscopy, robotic surgery, and open laparotomy.
4. Patient Selection and Counseling
The guidelines emphasize that OS should be discussed with all women who have completed childbearing and are undergoing relevant abdominal or pelvic surgery. This includes women undergoing benign gynecological surgeries (like hysterectomy for fibroids) and those seeking permanent sterilization. Interestingly, the consensus also suggests considering OS during non-gynecological surgeries, such as colorectal procedures or cholecystectomies, provided the surgical team is qualified and the patient is properly counseled.
Patient Vignette: Applying the Guidelines
Consider the case of **Sarah**, a 43-year-old woman in Chicago undergoing a laparoscopic hysterectomy for symptomatic uterine fibroids. Sarah has no family history of breast or ovarian cancer and is not a carrier of the BRCA mutation. Historically, a surgeon might have suggested leaving her fallopian tubes intact since she was at “average risk.”
Under the new ESGO consensus, Sarah’s surgeon would provide preoperative counseling on the benefits of opportunistic salpingectomy. The surgeon explains that since the tubes no longer serve a reproductive purpose for her, removing them can lower her lifetime risk of ovarian cancer without causing the hot flashes or bone density loss associated with menopause. Sarah chooses to proceed with the OS. The procedure adds 12 minutes to her surgery, and she recovers at the same rate as a standard hysterectomy patient, now with an added layer of cancer protection.
Expert Commentary and Insights
The ESGO panel highlighted several areas of expert agreement and a few points of ongoing discussion. One area of strong consensus was the inclusion of a patient representative in the working group. This ensured that the recommendations were not just clinically sound but also addressed the concerns and values of the women receiving the care.
**Dr. Jan M. Piek**, a lead author of the consensus, noted that while the procedure is highly effective for HGSOC, it does not eliminate the risk of all types of ovarian cancer (such as clear cell or endometrioid types which may have different origins). Therefore, OS should be framed as a risk-reduction strategy rather than an absolute guarantee of immunity.
There remains some controversy regarding the implementation of OS during non-gynecological surgeries. While the panel agreed it is feasible, they noted that the logistics of having a gynecologist available during a general surgery procedure, or training general surgeons to perform salpingectomy safely, remains a hurdle for many healthcare systems.
Practical Implications
For clinicians, the ESGO consensus shifts the burden of proof. It is no longer a question of “Why should we remove the tubes?” but rather “Is there a reason *not* to remove them?” in women who have completed childbearing.
Table 1: Summary of Recommendation Grades
| Domain | Recommendation | Grade |
|---|---|---|
| Risk Reduction | OS should be offered to lower the risk of HGSOC. | B |
| Ovarian Reserve | OS does not harm short-term ovarian function. | B |
| Non-Gyn Surgery | Consider OS during non-gynecological abdominal surgery. | D |
| Counseling | Shared decision-making must occur preoperatively. | C |
As these guidelines are integrated into hospital protocols, we expect to see a decrease in the incidence of tubo-ovarian cancer over the next two decades. This simple, “opportunistic” addition to routine surgeries represents one of the most promising public health interventions in modern gynecological oncology.
References
1. Piek JM, Schauwaert J, Ellis LB, et al. Opportunistic Salpingectomy for Prevention of Tubo-Ovarian Carcinoma: The European Society of Gynaecological Oncology Consensus Statements. JAMA. 2026;335(5):e2524510. doi:10.1001/jama.2025.24510.
2. Falconer H, Yin L, Grönberg H, Altman D. Ovarian cancer risk after salpingectomy: a nationwide population-based study. Journal of the National Cancer Institute. 2015;107(2):dju410.
3. Labidi-Galy SI, Papp E, Hallberg D, et al. High grade serous ovarian carcinomas originate in the fallopian tube. Nature Communications. 2017;8(1):1093.
4. McAlpine JN, Hanley GE, Woo MM, et al. Opportunistic salpingectomy: uptake, risks, and effectiveness of a strategy for ovarian cancer prevention. American Journal of Obstetrics and Gynecology. 2014;211(5):507.e1-507.e9.