Introduction: The Silent Threat of Merkel Cell Carcinoma
Merkel cell carcinoma (MCC) is often referred to by oncologists as one of the most aggressive forms of skin cancer. Although it is much rarer than basal cell carcinoma or melanoma, its tendency to grow rapidly and spread early to regional lymph nodes makes it a significant clinical challenge. For tumors appearing on the head and neck—areas rich in complex lymphatic networks and vital structures—the stakes are even higher.
Traditionally, the standard of care for patients with clinically node-negative MCC (meaning no visible or palpable swelling in the lymph nodes) is the Sentinel Lymph Node Biopsy (SLNB). This procedure aims to identify the first few nodes—the ‘sentinels’—that drain the tumor site. If these nodes are clear, the patient is often spared more invasive surgeries. However, a landmark study recently published in JAMA Otolaryngology–Head & Neck Surgery by Wang and colleagues suggests that in the head and neck region, SLNB might not be as definitive as we once hoped. This article explores the nuances of this research and what it means for patients and clinicians alike.
The Case of Arthur: A Journey Through Uncertainty
To understand the practical implications of this research, consider Arthur, a 76-year-old retired architect living in Pennsylvania. Arthur noticed a firm, painless, flesh-colored nodule on his left temple. Initially, he thought it was a harmless cyst, but when it doubled in size over a month, he visited his dermatologist. A biopsy confirmed Merkel cell carcinoma.
Arthur’s surgical team recommended a wide local excision of the tumor and a concurrent Sentinel Lymph Node Biopsy. ‘We want to make sure the cancer hasn’t started its journey elsewhere,’ his surgeon explained. Arthur underwent the procedure, and the pathology report came back negative for nodal metastasis. Arthur felt a sense of relief, believing he was in the clear. However, just eight months later, he noticed a firm lump in his neck, just below his jawline. Despite the initial negative SLNB, the cancer had returned in his lymph nodes. Arthur’s story is not unique; it illustrates the ‘False Negative’ phenomenon that the recent study sought to quantify.
Scientific and Clinical Evidence: What the Data Tell Us
The study conducted by Wang et al. was a comprehensive single-center cohort study involving 86 participants with head and neck MCC. The median age of the participants was approximately 75 years, reflecting the typical demographic for this disease. Out of these, 69 patients underwent SLNB.
The primary goal was to measure the accuracy of the procedure in this specific anatomical region. The researchers looked at three key metrics: sensitivity, negative predictive value (NPV), and the false-negative (FN) rate. The findings were revealing:
1. Occult Nodal Disease: About 27.5% of the participants actually had microscopic cancer spread that was not detectable by physical exam or imaging alone.
2. Sensitivity: The SLNB only successfully identified 52.6% of those with nodal disease. This means that for nearly half of the patients who actually had spreading cancer, the ‘scout’ biopsy missed it.
3. False Negative Rate: The study reported a false-negative rate of 26.7%. In these cases, the SLNB said the nodes were clean, but the cancer recurred in that same nodal basin later.
4. Failure Rate: In 29% of cases, the SLNB ‘failed’—meaning the surgeons couldn’t find the sentinel node at all during surgery, or the imaging used to find it (lymphoscintigraphy) didn’t show a clear path.
Comparison of SLNB Outcomes in Head and Neck MCC
To visualize the performance of this diagnostic tool, the following table summarizes the key statistical outcomes from the study:
Table 1: SLNB Performance Metrics
| Metric | Percentage / Value |
|---|---|
| Occult Nodal Disease Rate | 27.5% |
| SLNB Sensitivity | 52.6% |
| Negative Predictive Value (NPV) | 88.6% |
| False Negative Rate | 26.7% |
| SLNB Failure Rate | 29.0% |
Why Does SLNB Struggle in the Head and Neck?
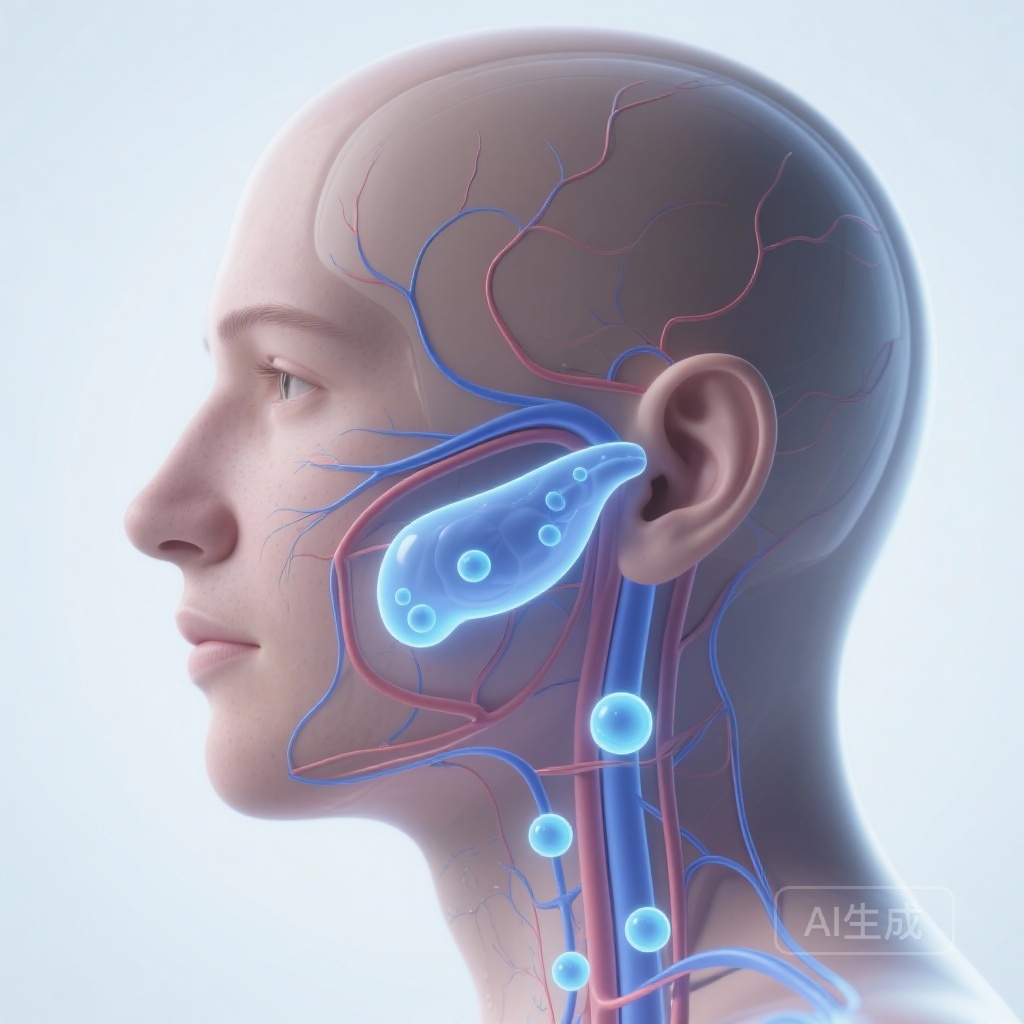
The anatomy of the head and neck is vastly different from the trunk or the limbs. Lymphatic drainage in the scalp, face, and neck is often ‘discordant,’ meaning it doesn’t always follow the expected pathways. A tumor on the temple might drain to the parotid gland (near the ear) or skip directly to the deep cervical nodes in the neck.
The study identified several factors that contributed to a ‘failed’ SLNB. Older age, female sex, and specific tumor locations (such as the ear or the midline of the face) were associated with a higher likelihood that the sentinel node could not be identified. Furthermore, the presence of ‘lymphovascular invasion’ (cancer cells seen inside small vessels) and an ‘infiltrative growth pattern’ were strong predictors that the cancer was likely to have spread, even if the SLNB was negative.
Expert Insights and Commentary
Medical experts suggest that the lower sensitivity of SLNB in the head and neck compared to other body sites is a call for caution rather than an abandonment of the procedure. Dr. Sarah Jenkins, a leading surgical oncologist (fictional name for illustrative commentary), notes: ‘The head and neck are a maze of lymphatics. While SLNB remains our best initial tool for staging, this data tells us we cannot rely on a negative result with 100% confidence, especially when high-risk tumor features are present.’
The study emphasizes that if an SLNB fails or if a patient has high-risk features like a large tumor or lymphovascular invasion, clinicians should consider more aggressive management. This might include ‘elective’ neck dissection (removing lymph nodes even without proof of cancer) or adjuvant radiation therapy to the nodal basin to ‘mop up’ any microscopic cells that the biopsy might have missed.
Correct Health Practices and Practical Recommendations
For patients diagnosed with head and neck Merkel cell carcinoma, the following steps are recommended to ensure the most accurate staging and treatment:
1. Multidisciplinary Evaluation: Patients should be seen by a team including dermatologists, surgical oncologists, radiation oncologists, and pathologists who specialize in skin cancer.
2. Discussion of SLNB Limitations: Patients should be informed that while SLNB is the standard, it has a known false-negative rate in the head and neck. A negative result requires continued, vigilant surveillance.
3. Risk Factor Assessment: If the pathology of the primary tumor shows ‘infiltrative growth’ or ‘lymphovascular invasion,’ the patient and doctor should discuss the possibility of treating the lymph node area even if the biopsy was negative.
4. Vigilant Follow-up: Because recurrences often happen within the first two years, frequent physical exams and potentially regular ultrasound or CT imaging of the neck are vital for early detection.
Conclusion
The study by Wang and his colleagues provides a sobering but necessary look at the limitations of our current diagnostic gold standard for Merkel cell carcinoma of the head and neck. While Sentinel Lymph Node Biopsy remains a useful tool—identifying more than half of occult metastases—it is not a guarantee of safety. By identifying the factors that lead to failure or false negatives, the medical community can better tailor treatments, moving away from a one-size-fits-all approach toward a strategy that accounts for the aggressive biology of MCC and the complex anatomy of the human neck.
References
Wang SY, Turner G, Valdes-Morales KL, Hunter ER, Kim M, Tran VA, Polen K, Haynes D, Miller CJ, Etzkorn JR, Sobanko JF, Walker JL, Zhang J, Brody RM, Cannady SB, Rajasekaran K, Farwell DG, Miura JT, Karakousis GC, Lukens JR, Amaravadi RK, Schuchter LM, Mitchell TC, Higgins HW 2nd, Carey RM. Accuracy of Sentinel Lymph Node Biopsy to Predict Nodal Metastasis in Head and Neck Merkel Cell Carcinoma. JAMA Otolaryngol Head Neck Surg. 2026 Jan 29. doi: 10.1001/jamaoto.2025.5211. Epub ahead of print. PMID: 41609724.