Highlight
– Platelet transfusions were given to 6% of critically ill adults across 233 centres in 30 countries, primarily for active bleeding or prophylaxis.
– Median pretransfusion platelet count was 44 × 10^9/L, with higher counts before transfusion for active bleeding (median 60 × 10^9/L).
– A stated transfusion threshold was recorded for only half of events and was not adhered to in 16% of cases; practice varied substantially by geo-economic region.
Background
Thrombocytopenia and bleeding are common problems in critically ill patients and are associated with increased morbidity and mortality. Platelet transfusion is the principal therapeutic intervention for severe thrombocytopenia or platelet dysfunction when clinicians judge bleeding risk to be unacceptably high. However, platelet transfusions carry costs and risks — transfusion reactions, alloimmunization, transfusion-transmitted infection, and volume/immune-mediated complications — and the evidence base for specific transfusion thresholds in the heterogeneous intensive care unit (ICU) population remains limited. International guidelines provide recommendations for some clinical scenarios (for example, prophylaxis in profound thrombocytopenia and periprocedural thresholds), but practice is often extrapolated from oncology, surgery, or haemostasis literature rather than generated from contemporary ICU-focused randomized trials.
Study design
This prospective, multicenter cohort study (the InPUT Study Group) enrolled all adult patients (aged ≥18 years) admitted during a predetermined study week at each of 233 participating centres across 30 countries between March 2019 and October 2022. There were no interventions. Investigators recorded whether patients received platelet transfusions during their ICU stay and documented the indication (active bleeding, prophylaxis, procedure-related, other), pretransfusion platelet count, whether a transfusion threshold was specified by the treating team, adherence to advised thresholds, and geo-economic region (classified by income level). The primary objective was to describe platelet transfusion occurrence and practice patterns, including thresholds and adherence; secondary analyses examined regional variation.
Key findings
Population and overall use
– Among 3,643 ICU patients, 208 (6%) received at least one platelet transfusion during their ICU stay.
– A total of 443 platelet transfusion events were analyzed (multiple transfusions per patient possible).
Indications
– Active bleeding accounted for the largest proportion of transfusion events (42%, 187/443).
– Prophylactic transfusions (intended to reduce bleeding risk without active bleeding) comprised 33% (144/443).
– Transfusions given for an upcoming procedure were 12% (51/443); the remainder were for other or undocumented indications.
Pretransfusion platelet counts and thresholds
– Median platelet count before transfusion across all events was 44 × 10^9/L (interquartile range [IQR] 20–78 × 10^9/L).
– Counts varied by indication: during active bleeding the median was higher at 60 × 10^9/L (IQR 31–93), reflecting clinician preference to transfuse at higher counts in bleeding patients; prophylactic transfusions tended to occur at lower counts.
– A specific transfusion threshold was explicitly documented in 51% of transfusion events (224/443). The median stated threshold was 50 × 10^9/L (IQR 40–100).
– When a threshold was documented, it was not followed in 16% of events (36/224). Most instances of non-adherence involved active bleeding as the indication, where clinicians often deviate from fixed thresholds to address dynamic haemorrhage risk.
Geo-economic variation
– Platelet transfusion use differed by regional income level: 6% of patients in high-income countries received platelets (156/2,520), 5% in upper-middle-income countries (52/1,069), and none in lower-middle-income countries (0/54) within the sample.
– Non-adherence to stated thresholds was more common in high-income settings (23%, 34/149) compared with upper-middle-income settings (3%, 2/75).
– These differences likely reflect variation in resource availability, transfusion culture, clinician training, procedure mix, and case-mix severity, as well as sample size and site representation from lower-income regions.
Clinical implications of the findings
– Platelet transfusions are relatively infrequent in ICUs but are concentrated around bleeding and procedural risk mitigation. The median pretransfusion platelet counts and stated thresholds cluster around commonly recommended values (e.g., 50 × 10^9/L), yet considerable heterogeneity remains.
– The finding that single-center guidance was documented only half the time suggests either lack of explicit local rules for platelet practice in many ICUs or failure to record the rationale. Non-adherence in bleeding scenarios likely reflects appropriate clinical judgment in dynamic situations but could also indicate inconsistent application of policies.
Expert commentary and contextualization
How does this align with guideline recommendations?
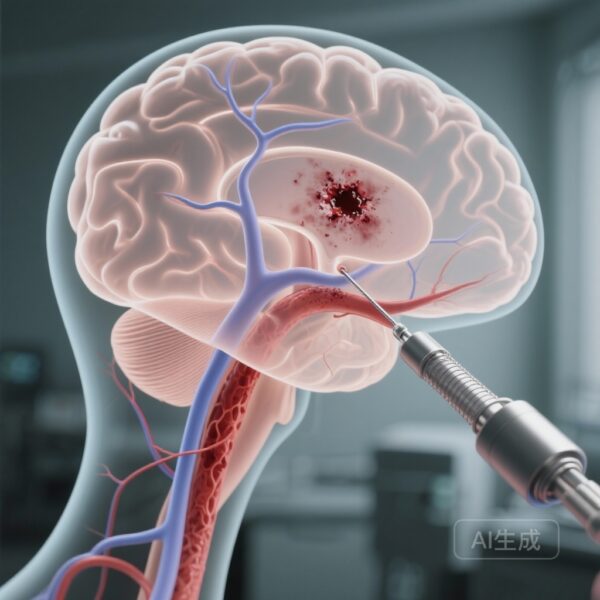
– Existing guideline documents provide context-specific platelet thresholds: for example, many societies recommend maintaining platelet counts ≥50 × 10^9/L for most major bleeding or invasive procedures, ≥100 × 10^9/L for central nervous system procedures, and prophylactic transfusion for severe thrombocytopenia (commonly <10 × 10^9/L in haematology patients). However, those recommendations derive largely from non-ICU populations or expert consensus, and extrapolation to critically ill patients — who often have complex coagulopathies, consumptive processes, sepsis-associated platelet dysfunction, or extracorporeal circuits — is imperfect.
Mechanistic and practical considerations
– Platelet transfusion decisions in the ICU require integrating the platelet count with clinical bleeding, ongoing anticoagulation or antiplatelet therapy, procedural urgency, and dynamic haemorrhage risk. Traditional platelet counts do not capture platelet function, and point-of-care viscoelastic testing (TEG/ROTEM) or platelet function assays can offer additional information but are not universally available.
Risk-benefit balance and stewardship
– Given costs and risks, transfusion stewardship is important. The low overall transfusion rate in this cohort argues that indiscriminate platelet use is not widespread but the observed regional variability and incomplete documentation indicate opportunities for targeted stewardship interventions: defining local indications, improving documentation, audit and feedback, and use of decision-support tools.
Evidence gaps and research priorities
– There is a paucity of randomized controlled trials that test platelet transfusion thresholds specifically in heterogeneous ICU populations. Pragmatic, context-specific trials (for example, comparing restrictive vs. liberal platelet thresholds in bleeding vs. non-bleeding ICU patients, or trials targeting procedure-specific thresholds) are needed. Trials incorporating functional haemostasis testing and patient-centred outcomes (bleeding, transfusion reactions, mortality, resource use) would be particularly valuable.
Limitations
Interpretation of this study should consider several limitations. The sampling method (one study week per site) provides a cross-sectional snapshot that may not capture seasonal or case-mix variability. Centers self-selected their study week from predefined options, which could introduce selection bias. Representation from lower-middle-income countries was small (n=54 patients), limiting conclusions in those settings. Documentation of thresholds occurred in only half of events, reducing the power of adherence analyses. Finally, the study was observational and cannot determine whether transfusions were beneficial or harmful in individual cases.
Conclusion and practical takeaways
This large international prospective cohort shows that platelet transfusions in the ICU are uncommon (6% of patients) and most often used for active bleeding or prophylaxis. Median pretransfusion platelet counts centered around 44 × 10^9/L overall and 60 × 10^9/L during bleeding, with many centers advising thresholds near 50 × 10^9/L. However, documentation and adherence to thresholds were inconsistent, and substantial geo-economic variation exists. These findings highlight the need for improved documentation, context-sensitive transfusion stewardship, and randomized trials to define optimal platelet transfusion strategies in critically ill populations.
Practical recommendations for clinicians
– Explicitly document the indication and threshold (if any) when ordering platelet transfusion to support audit and stewardship.
– Apply higher transfusion targets when major bleeding or high-risk procedures (especially CNS procedures) are present, and consider platelet function and anticoagulant status when available.
– Engage transfusion medicine and haemostasis specialists for complex cases, and consider point-of-care tests where available to guide targeted therapy.
– Participate in or support pragmatic trials and multicentre registries to close evidence gaps.
Funding and trial registry
See the original publication for details on funding and trial registration: van Wonderen SF et al., Crit Care Med. 2025.
References
1. van Wonderen SF, Raasveld SJ, Flint AWJ, et al.; InPUT Study Group. Platelet Transfusion Practices in the ICU: A Prospective Multicenter Cohort Study. Crit Care Med. 2025 Dec 1;53(12):e2526-e2539. doi: 10.1097/CCM.0000000000006880.
2. Estcourt LJ, Birchall J, Allard S, et al. Guidelines for the use of platelet transfusions. British Journal of Haematology. 2017;176(3):365–394. (BCSH Guideline)
Where to find more
Readers interested in operationalizing findings should review local and national transfusion guidelines, engage their transfusion committees, and consider multi-disciplinary quality-improvement projects to standardize documentation and indication-specific pathways for platelet use in the ICU.