Study Background and Disease Burden
Percutaneous coronary intervention (PCI) is a widely employed revascularization procedure in patients with stable ischemic heart disease to alleviate symptoms and improve outcomes. However, myocardial injury frequently occurs peri-procedurally, reflected by biomarker elevation, and is increasingly recognized as a marker of worse prognosis. Creatine kinase myocardial band (CKMB) elevation after PCI identifies myocardial injury distinct from acute myocardial infarction. Despite this, predictors for post-PCI myocardial injury are heterogeneous and not fully elucidated. Furthermore, the long-term prognostic significance of myocardial injury based on CKMB elevation after elective PCI remains controversial. Understanding the incidence, clinical associations, and long-term consequences of post-PCI myocardial injury may inform patient risk stratification and management. This study from NYU Langone Health addresses these important gaps by evaluating a large cohort undergoing elective PCI and assessing post-procedural CKMB elevations and associated mortality outcomes over extended follow-up.
Study Design
A retrospective observational study included consecutive adults aged 18 years and older with stable ischemic heart disease who underwent elective PCI at NYU Langone Health between 2011 and 2020. Patients presenting with acute myocardial infarction or baseline CKMB or troponin levels exceeding the 99th percentile of the upper reference limit prior to PCI were excluded to avoid confounding from preexisting injury. CKMB concentrations were routinely measured at 1 and 3 hours post-procedure. Post-PCI myocardial injury was defined by a peak CKMB concentration exceeding the 99% upper reference limit post-PCI. Clinical factors were examined for association with this injury using linear regression models, while Cox proportional hazards models evaluated the relationship between post-PCI myocardial injury and all-cause mortality during long-term follow-up. This extensive dataset provided robust power to evaluate predictors and long-term outcomes with comprehensive adjustment for covariates.
Key Findings
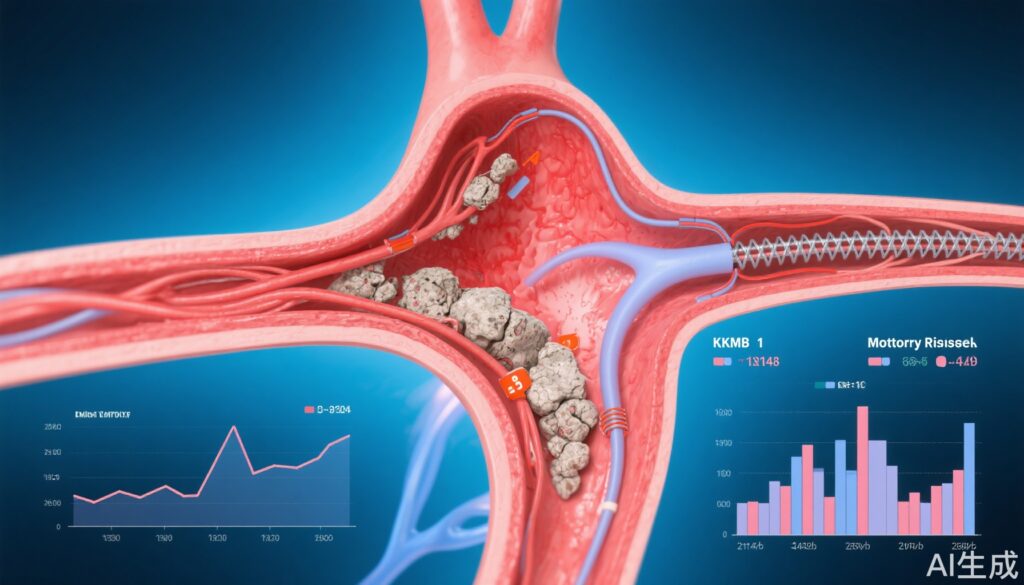
Among 10,807 elective PCI patients (median age 67 years; 24.9% female), post-PCI myocardial injury occurred in 1,813 patients, representing 16.8% of the cohort. Notably, myocardial injury was less frequent among females than males (14.1% vs. 17.7%, P<0.001). Several clinical and procedural characteristics independently associated with post-PCI myocardial injury were identified: older age, longer coronary lesion length, multivessel PCI procedures, severe coronary artery calcification, and use of thrombectomy devices correlated with remarkable increases in CKMB levels exceeding the upper reference limit.
Over a mean follow-up period of 4.3 years, covering 46,071 patient-years, 472 patients died (4.4%). Mortality was significantly higher in patients experiencing post-PCI myocardial injury compared with those without injury (7.9% vs. 3.6%, P<0.001). Adjusted Cox regression analysis demonstrated that post-PCI myocardial injury was independently associated with increased long-term all-cause mortality (hazard ratio 1.46; 95% CI, 1.20–1.78) after accounting for demographic and clinical covariates. These results highlight the clinical importance of recognizing myocardial injury detected by CKMB elevation after elective PCI.
Expert Commentary
This study robustly confirms that even minor elevations in CKMB after elective PCI—indicative of myocardial injury—carry significant prognostic implications for long-term survival. The associations with procedural complexity elements such as lesion length, multivessel interventions, and heavy coronary calcification underscore the impact of anatomical factors and procedural challenges on myocardial insult. The sex difference in injury incidence calls for further exploration of underlying biological or procedural susceptibilities. While CKMB remains a classical marker of myocardial injury, integrating newer high-sensitivity troponin assays and imaging modalities may provide additional risk stratification precision.
These findings align with evolving guidelines emphasizing procedural optimization to minimize myocardial injury. However, current optimal management strategies for patients identified with post-PCI myocardial injury remain incompletely defined. Further prospective studies incorporating mechanistic insights and evaluating targeted interventions are warranted to improve outcomes.
Conclusion
Myocardial injury detected by elevated CKMB early post-elective PCI is common, occurring in nearly one-sixth of patients, and is independently associated with increased risk of all-cause long-term mortality. More complex coronary anatomy and intervention characteristics predict heightened myocardial injury risk. This study underscores the prognostic importance of routine post-PCI CKMB monitoring and highlights the need for heightened clinical vigilance and possibly tailored management strategies in patients experiencing periprocedural myocardial injury. Further research is needed to refine therapeutic approaches to mitigate this risk and improve cardiovascular outcomes after elective PCI.
References
Talmor N, Graves C, Kozloff S, Major VJ, Xia Y, Shah B, Babaev A, Razzouk L, Rao SV, Attubato MJ, Feit F, Slater J, Smilowitz NR. Periprocedural Myocardial Injury Using CKMB Following Elective PCI: Incidence and Associations With Long-Term Mortality. Circ Cardiovasc Interv. 2025 May;18(5):e014934. doi: 10.1161/CIRCINTERVENTIONS.124.014934. Epub 2025 Mar 31. PMID: 40160098; PMCID: PMC12092176.