Introduction: The Evolving Landscape of Metabolic Dysfunction-Associated Steatohepatitis
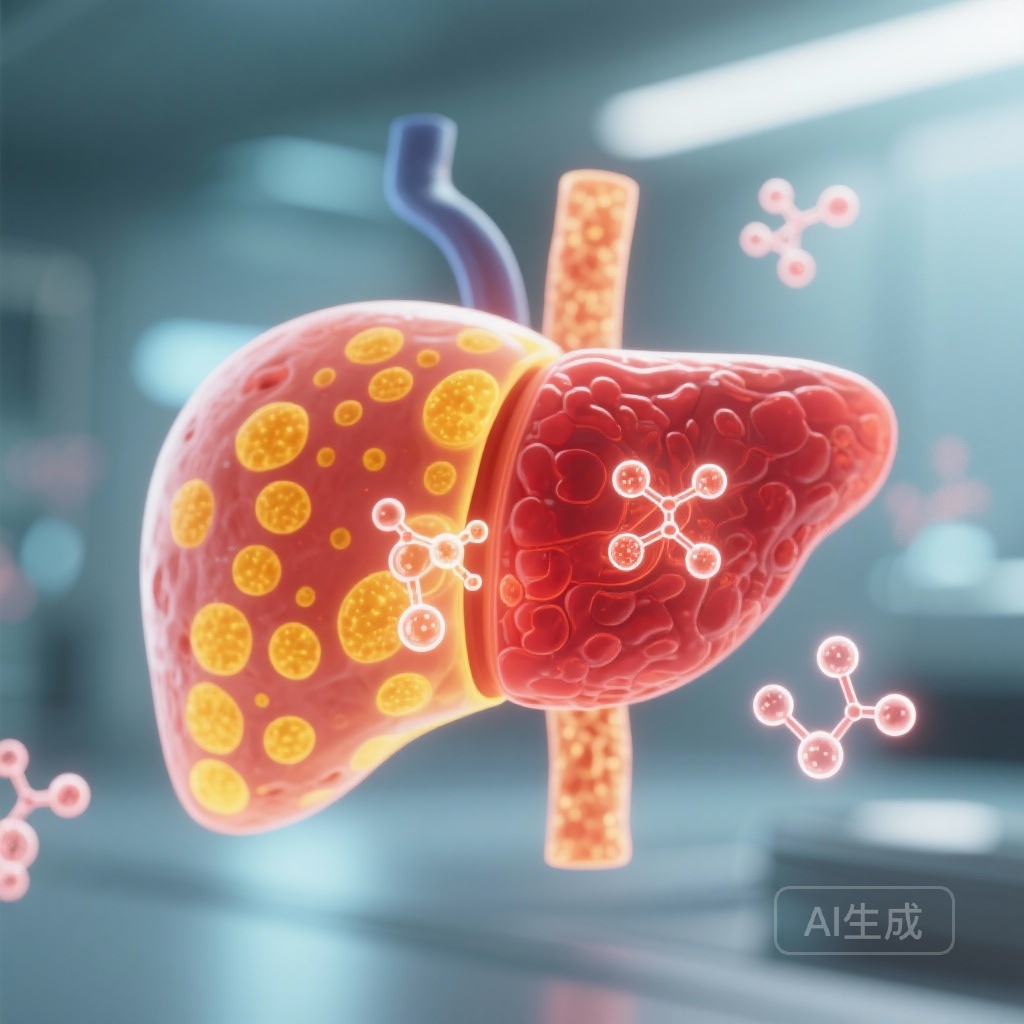
Metabolic dysfunction-associated steatohepatitis (MASH), formerly known as non-alcoholic steatohepatitis (NASH), has emerged as a global health crisis, paralleling the rise in obesity and type 2 diabetes. As the leading cause of chronic liver disease and a rapidly growing indication for liver transplantation, MASH represents a significant unmet medical need. The pathophysiology of MASH is complex, involving a ‘multi-hit’ process of lipid accumulation, oxidative stress, and inflammatory signaling that ultimately leads to progressive fibrosis and cirrhosis.
Current therapeutic strategies are shifting toward agents that address both the underlying metabolic drivers and the downstream hepatic consequences. While the recent FDA approval of resmetirom marked a milestone, there remains a demand for therapies with more potent metabolic effects and weight-loss benefits. In this context, pemvidutide, a novel GLP-1 and glucagon dual receptor agonist, has garnered significant attention. The 24-week results of the IMPACT trial provide a critical look at the efficacy and safety of this dual-action approach in patients with moderate-to-severe fibrosis.
The Mechanistic Rationale: Why GLP-1 and Glucagon?
Most current incretin-based therapies for MASH focus on the glucagon-like peptide-1 (GLP-1) receptor. GLP-1 agonists primarily work by enhancing glucose-dependent insulin secretion, delaying gastric emptying, and promoting satiety, which leads to weight loss and improved insulin sensitivity. However, pemvidutide adds a second layer of pharmacology: glucagon receptor agonism.
Glucagon is traditionally viewed as a counter-regulatory hormone to insulin, but in the context of MASH, its inclusion is strategic. Glucagon increases energy expenditure through thermogenesis and directly stimulates hepatic lipid metabolism by promoting mitochondrial beta-oxidation. By combining GLP-1’s appetite-suppressing effects with glucagon’s ability to ‘burn’ liver fat and increase caloric burn, pemvidutide aims to achieve a synergistic reduction in hepatic steatosis and systemic metabolic dysfunction.
Study Design and Methodology of the IMPACT Trial
The IMPACT trial (NCT05989711) is an ongoing 48-week, international, multicenter, randomised, double-blind, placebo-controlled, phase 2b study. The study specifically targeted a high-risk population: patients with biopsy-confirmed MASH and liver fibrosis stages F2 or F3, as defined by the NASH Clinical Research Network (CRN) scoring system. These patients represent the ‘sweet spot’ for clinical intervention, where the risk of progression to cirrhosis is high, but the potential for reversal remains significant.
Participants (n=212) from 83 sites in the USA and Australia were randomized in a 1:2:2 ratio to receive once-weekly subcutaneous injections of either placebo, 1.2 mg pemvidutide, or 1.8 mg pemvidutide. A unique feature of this trial was the administration of pemvidutide without dose titration—a departure from the standard escalation protocols required for most GLP-1 based therapies. The dual primary endpoints were measured at the 24-week mark: (1) MASH resolution without worsening of fibrosis and (2) at least a one-stage improvement in liver fibrosis without worsening of MASH.
Key Findings: A Deep Dive into the 24-Week Data
MASH Resolution: A Clear Statistical Victory
The 24-week interim analysis revealed a striking difference in MASH resolution rates. In the placebo group, only 20% (18/86) of patients achieved resolution. In contrast, 58% (24/41) of patients in the 1.2 mg pemvidutide group (p<0.0001) and 52% (45/85) in the 1.8 mg pemvidutide group (p<0.0001) met the endpoint. This represents a therapeutic gain of 38% and 32%, respectively, over placebo.
These results suggest that pemvidutide is highly effective at clearing hepatic fat and resolving the inflammatory components of MASH (ballooning and lobular inflammation) within a relatively short timeframe. The achievement of over 50% resolution in a population with advanced fibrosis (F2-F3) is particularly noteworthy compared to historical data from GLP-1 mono-agonists.
Fibrosis Improvement: The Challenge of Timing
While the resolution data was robust, the study did not meet its other primary endpoint of fibrosis improvement at 24 weeks. Fibrosis improvement of at least one stage without worsening of MASH was observed in 28% of the placebo group, 33% of the 1.2 mg group (p=0.59), and 36% of the 1.8 mg group (p=0.27). While numerically higher in the treatment arms, the differences did not reach statistical significance.
Clinical experts suggest that 24 weeks may simply be too short to observe structural remodeling of the extracellular matrix in patients with established F2 or F3 fibrosis. Fibrosis regression is a slower biological process than the resolution of inflammation and steatosis. The ongoing 48-week data will be crucial in determining whether the rapid resolution of MASH eventually translates into significant fibrosis reduction over a longer duration.
Safety and Tolerability: A Favorable Profile Without Titration
The safety profile of pemvidutide is a critical consideration, especially given the lack of dose titration. Adverse events (AEs) were reported in 78-81% of pemvidutide-treated patients compared to 67% in the placebo group. As expected with this class of drug, the majority of AEs were gastrointestinal in nature, including nausea and vomiting. However, most events were characterized as mild or moderate.
Perhaps most impressively, the discontinuation rate due to AEs was remarkably low: 0% in the 1.2 mg group and only 1% in the 1.8 mg group, compared to 2% in the placebo group. This suggests that the dual-agonist approach, even without titration, is well-tolerated by patients with MASH, potentially offering a more streamlined clinical implementation than drugs requiring months of dose escalation.
Expert Commentary and Clinical Interpretation
The IMPACT trial results underscore the potency of dual GLP-1/glucagon agonism in treating the ‘active’ phase of MASH. By targeting the liver through two distinct pathways, pemvidutide appears to accelerate the clearance of inflammation. The lack of statistical significance in fibrosis at 24 weeks should be interpreted with caution; in many MASH trials, fibrosis improvement is a ‘lagging indicator’ that follows MASH resolution.
From a health policy and clinical practice perspective, pemvidutide’s ability to achieve these results without titration could simplify the treatment journey for both providers and patients. Furthermore, the weight loss observed with pemvidutide (a known secondary benefit of this molecule) provides a comprehensive metabolic benefit that mono-targeted therapies may lack.
However, limitations must be acknowledged. The 24-week duration is an interim look, and the long-term durability of these effects remains to be seen. Additionally, while the safety profile is encouraging, the long-term effects of chronic glucagon agonism on cardiovascular parameters and glucose homeostasis in diabetic vs. non-diabetic MASH populations require continued monitoring.
Conclusion: Looking Toward the 48-Week Horizon
In summary, the 24-week results of the IMPACT trial demonstrate that pemvidutide is a highly effective inducer of MASH resolution in patients with F2 and F3 fibrosis. While the fibrosis improvement endpoint was not met at this early interval, the magnitude of MASH resolution and the excellent tolerability profile support the continued development of pemvidutide. The medical community eagerly awaits the 48-week data, which will provide the definitive evidence needed to determine if this dual agonist can indeed reverse the structural damage of liver fibrosis. For now, pemvidutide stands as a promising candidate in the rapidly expanding pharmacopeia for metabolic liver disease.
Funding and Trial Information
This study was funded by Altimmune. ClinicalTrials.gov Identifier: NCT05989711.
References
Noureddin M, Harrison SA, Loomba R, et al. Safety and efficacy of weekly pemvidutide versus placebo for metabolic dysfunction-associated steatohepatitis (IMPACT): 24-week results from a multicentre, randomised, double-blind, phase 2b study. Lancet. 2025;406(10520):2644-2655. doi:10.1016/S0140-6736(25)02114-2.