Highlights
– A nucleoside‑modified mRNA (modRNA) influenza vaccine, given 30 days before challenge, prevented symptomatic and febrile A/H1N1 illness in a human challenge model (VE 100% vs control; 95% CI lower bounds 75.2% and 61.2% respectively).
– Both the modRNA vaccine and licensed quadrivalent inactivated influenza vaccine (QIV) reduced viral shedding (VL‑AUC and peak viral load) compared with unvaccinated controls; reductions were larger for modRNA versus QIV.
– No serious adverse events were reported; sample size and challenge model limit generalizability to older or high‑risk populations and to field effectiveness against circulating strains.
Background and Unmet Need
Seasonal influenza remains a substantial public health burden worldwide despite widespread vaccination programs. Conventional influenza vaccines (egg‑ or cell‑based inactivated, live attenuated) have variable effectiveness year to year because of antigenic drift, egg‑adaptation, and the need for frequent reformulation. Nucleoside‑modified messenger RNA (modRNA) platforms, which have been brought to clinical prominence by SARS‑CoV‑2 vaccines, promise rapid manufacturability, potent immunogenicity, and flexible antigen design. However, direct evidence of clinical protection after human exposure to influenza virus for modRNA influenza vaccines had not been reported in a controlled human challenge model until the trial summarized here.
Study Design
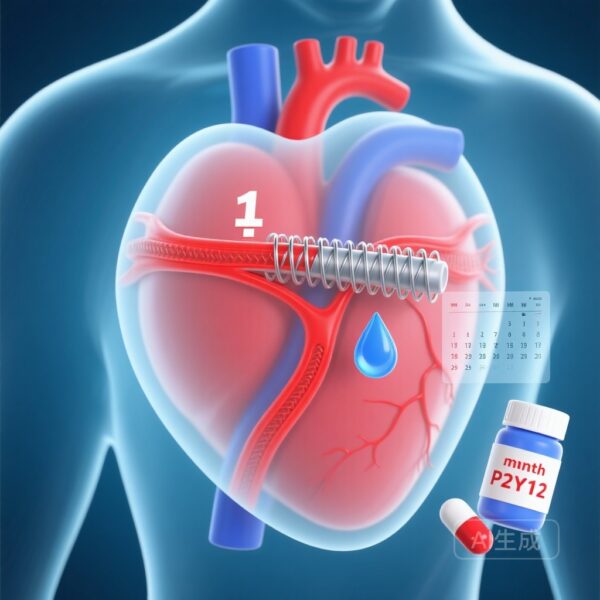
This randomized, double‑blind, phase 2a human challenge trial enrolled healthy adults 18–55 years old and randomized them 1:1 to receive either a modRNA influenza vaccine or a licensed quadrivalent influenza vaccine (QIV) 30 days before intranasal challenge with influenza A/H1N1. A contemporaneous unvaccinated control cohort was taken from a separate trial cohort exposed to the same challenge strain to facilitate efficacy comparisons.
Primary efficacy assessments considered events occurring from day 1 to day 8 postchallenge and included four co‑primary endpoints: two binary clinical endpoints and two virologic endpoints. The clinical endpoints were (1) laboratory‑confirmed symptomatic influenza of at least grade 2 severity and (2) febrile influenza (temperature ≥37.9°C). The virologic endpoints were median differences between vaccine and control groups for (3) area under the viral load–time curve (VL‑AUC) and (4) peak viral load (peak VL). Vaccine efficacy (VE) for clinical endpoints was calculated as 1 minus the relative risk versus control.
The per‑protocol analysis included 55 participants in the modRNA arm, 48 in the QIV arm, and 52 unvaccinated controls. Safety endpoints included solicited local and systemic reactions and serious adverse events (SAEs).
Key Results
Clinical Efficacy
In the per‑protocol cohort, laboratory‑confirmed symptomatic influenza occurred in 0% (0/55) of modRNA recipients, 4.2% (2/48) of QIV recipients, and 26.9% (14/52) of unvaccinated controls. The calculated VE against symptomatic illness was 100.0% (95% CI, 75.2% to 100.0%) for the modRNA vaccine and 84.5% (95% CI, 43.4% to 96.0%) for QIV compared with controls.
Febrile influenza (temperature ≥37.9°C) occurred in 0% of both vaccine groups and 17.3% (9/52) of controls, yielding VE estimates of 100.0% (95% CI, 61.2% to 100.0%) for the modRNA vaccine and 100.0% (95% CI, 55.9% to 100.0%) for QIV.
Interpretation: Both vaccines substantially reduced the risk of symptomatic and febrile illness after controlled A/H1N1 exposure, with the modRNA vaccine showing a point estimate of complete protection in this sample. Confidence intervals, particularly for the QIV comparisons, are wide and reflect relatively small sample sizes and low event counts in vaccine arms.
Virologic Endpoints
The modRNA vaccine was associated with larger reductions in viral replication metrics compared with control and with larger median differences than QIV. Median differences in VL‑AUC between vaccine and control were −88.66 for the modRNA (95% CI, −261.95 to −1.35) and −67.01 for QIV (95% CI, −254.13 to −0.97). Median differences in peak viral load were −4.52 for modRNA (95% CI, −5.29 to 0.00) and −1.49 for QIV (95% CI, −5.25 to 0.00).
Interpretation: The modRNA vaccine significantly reduced cumulative viral shedding and had a larger effect on peak viral load than QIV in this challenge context. Reduced viral load is biologically plausible as a mechanism for reduced symptoms and transmissibility, although the short window of observation (days 1–8) limits conclusions about full shedding duration.
Safety
No serious adverse events were reported in any group. The report did not indicate unexpected safety signals within the sample size and follow‑up duration. As with other early vaccine studies, the sample consisted of healthy adults 18–55 years, a population at low risk for vaccination complications; safety in older adults or medically vulnerable populations remains to be established.
Strengths of the Study
– Controlled exposure model: Human challenge trials allow precise timing and uniform infectious dose, improving sensitivity to detect vaccine effects on clinical illness and virologic outcomes compared with field trials.
– Head‑to‑head comparison with a licensed influenza vaccine (QIV) provides a practical benchmark for interpreting effect sizes.
– Multiple endpoints capturing both clinical and virologic outcomes strengthen inferences about both symptomatic protection and effects on viral replication.
Limitations and Considerations
– Generalizability: Challenge trials enroll healthy young adults and use a single, characterized challenge strain. These features limit extrapolation to older adults, children, pregnant people, or those with comorbidities, and to protection against antigenically drifted or heterologous strains circulating in the community.
– Timing and durability: Vaccination occurred 30 days before challenge, measuring short‑term protection. The trial does not address durability of protection over months or across seasons.
– Sample size and CIs: The numbers of clinical endpoint events in vaccine arms were small (zero events in modRNA), producing point estimates of 100% VE with wide confidence intervals. While encouraging, these estimates should be confirmed in larger field efficacy trials.
– Immune correlates: The published summary focuses on clinical and virologic endpoints; detailed immunogenicity data (neutralizing antibodies, hemagglutination inhibition titers, mucosal immunity, cellular responses) are needed to establish correlates of protection and to guide regulatory evaluation and future immunobridging studies.
– Challenge strain relevance: The A/H1N1 challenge strain may not reflect antigenic properties of contemporary seasonal strains; effectiveness against drifted viruses or different subtypes (e.g., A/H3N2) remains unknown.
– External control group: Controls came from a separate trial exposed to the same virus; while methods aimed for comparability, randomized contemporaneous placebo controls would be the gold standard to avoid subtle selection or procedural differences.
Clinical and Public Health Implications
This human challenge trial provides proof‑of‑concept that a nucleoside‑modified mRNA influenza vaccine can prevent symptomatic and febrile illness after controlled A/H1N1 exposure and reduce viral replication more than a licensed QIV in healthy adults. If replicated in larger field trials and across age groups and antigenic subtypes, modRNA platforms could offer important advantages: rapid strain updates, scalable manufacturing, and potentially higher or broader immunogenicity.
Reduced viral shedding after vaccination could also translate into lower secondary transmission, an important population‑level benefit that would require community studies to confirm.
Next Steps and Research Priorities
– Conduct randomized, adequately powered field efficacy trials across age groups, including older adults and high‑risk populations, to measure real‑world effectiveness and safety.
– Characterize immunogenicity comprehensively (serologic and mucosal antibodies, T‑cell responses) and identify correlates of protection that support immunobridging and regulatory pathways.
– Test modRNA formulations against multiple contemporary influenza strains and in multivalent constructs representative of seasonal vaccines, including assessment of antigenic breadth and cross‑protection.
– Evaluate durability of protection over months and across influenza seasons, and assess booster strategies.
– Investigate the effect of vaccination on viral transmission in household or community studies.
Expert Commentary
Human challenge trials are uniquely informative for early efficacy signals and mechanistic understanding but are complementary to—rather than substitutes for—field efficacy and population safety studies. The strong virologic and clinical protection seen with the modRNA vaccine in this controlled exposure context is promising and aligns with the broader experience that mRNA platforms can elicit robust immune responses. However, regulatory and public health decisions will depend on larger trials demonstrating effectiveness across diverse populations and influenza seasons, and on robust safety data over longer follow‑up.
Conclusions
In this phase 2a human challenge study, a nucleoside‑modified mRNA influenza vaccine given 30 days before challenge prevented symptomatic and febrile A/H1N1 illness and reduced viral load compared with unvaccinated controls, with no serious adverse events identified. Results support advancement to larger field trials to assess breadth, durability, and safety across populations and influenza strains. If confirmed, modRNA influenza vaccines could represent an important advance in seasonal influenza prevention and pandemic preparedness.
Funding and Trial Registration
Funded by hVIVO and Pfizer. Clinical trial registration: ISRCTN13789612.
References
1. Lindert KA, Mann A, Geevarughese A, Hauguel T, Mirza S, Bevan M, Yi K, Wolfe K, Nantermet P, Eze K, Dokhe P, Zareba AM, Gomme E, Catchpole AP, Anderson AS, Gurtman A, Suphaphiphat Allen P. Human Challenge Trial of a Nucleoside‑Modified Messenger Ribonucleic Acid Influenza Vaccine. NEJM Evid. 2025 Dec;4(12):EVIDoa2500087. doi: 10.1056/EVIDoa2500087. Epub 2025 Nov 19. PMID: 41259791.
Note: This article summarizes and interprets the above published trial results. Readers should consult the full publication for complete methods, statistical analyses, supplementary data, and author disclosures.