Highlights
Distinct Neuro-Immune Profiles
The PRONIA study identified separate multivariate signatures for early-stage depression and psychosis, involving specific cytokines and gray matter volume (GMV) alterations.
Differential Cytokine Involvement
Psychosis was characterized by elevated IL-6 and TNF-alpha with reduced CRP, whereas depression was associated with elevated IL-1beta, IL-2, IL-4, S100B, and BDNF.
Structural Specificity
Psychosis signatures mapped to corticothalamic circuits, while depression signatures involved limbic region reductions.
Environmental and Cognitive Drivers
Childhood trauma predicted both signatures, but cognitive performance was uniquely predictive of the psychosis signature.
Introduction: The Immunopsychiatry Paradigm Shift
For decades, the field of psychiatry has relied on symptom-based diagnostic categories that often overlap, leading to challenges in early intervention and personalized treatment. However, the emerging field of immunopsychiatry suggests that low-grade systemic inflammation and neuroanatomical changes may provide more objective biomarkers for these disorders. The central question addressed by the PRONIA (Personalized Prognostic Tools for Early Psychosis Management) consortium is whether these biological markers form distinct or shared patterns across early-stage mood and psychotic disorders. By integrating peripheral blood biomarkers with structural magnetic resonance imaging (MRI), researchers aimed to move beyond dimensional models toward a more biologically grounded understanding of mental illness.
Study Design and Methodology
The PRONIA study was a naturalistic, multicenter investigation conducted across eight sites in five European countries, including Germany, Italy, Switzerland, Finland, and the United Kingdom. Between February 2014 and May 2019, researchers recruited 678 participants, including individuals with recent-onset depression (ROD, n = 163), recent-onset psychosis (ROP, n = 177), clinical high-risk states for psychosis (CHR-P, n = 172), and healthy controls (HC, n = 166).
To ensure the results reflected primary pathophysiology rather than the effects of long-term treatment, the study focused on participants with minimal medication exposure. The researchers employed a sophisticated transdiagnostic machine learning approach, specifically sparse partial least squares (sPLS), to identify latent ‘brain-blood signatures.’ These signatures were derived from 11 peripheral assays—including cytokines like interleukin (IL)-6, IL-1beta, tumor necrosis factor (TNF)-alpha, C-reactive protein (CRP), and brain-derived neurotrophic factor (BDNF)—and structural MRI data measuring gray matter volume (GMV). Furthermore, support vector machine (SVM) classification was used to evaluate how psychosocial factors (such as childhood trauma) and neurocognitive performance predicted the expression of these biological signatures.
Key Findings: The Psychosis Signature
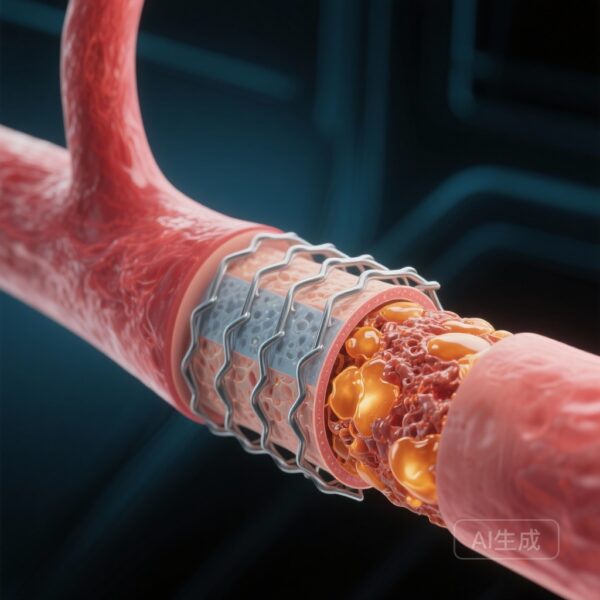
The analysis revealed a robust psychosis signature (correlation coefficient rho = 0.27; P = .002) that effectively differentiated individuals with ROP from those in the CHR-P phase. This signature was characterized by a specific peripheral inflammatory profile: elevated levels of the pro-inflammatory cytokines IL-6 and TNF-alpha, coupled with surprisingly reduced levels of CRP.
From a neuroanatomical perspective, this signature was associated with significant GMV shifts in the corticothalamic circuits. These circuits are critical for sensory gating and higher-order cognitive processing, and their disruption has long been hypothesized as a core feature of psychotic disorders. The fact that this signature could distinguish ROP from CHR-P suggests that the transition to full psychosis may involve a specific intensification of neuro-immune interaction within these circuits.
Key Findings: The Depression Signature
In contrast, the depression signature (rho = 0.19; P = .02) uniquely differentiated individuals with ROD from healthy controls. The biological profile of this signature was notably different from that of psychosis. It involved elevated levels of IL-1beta, IL-2, and IL-4, as well as higher concentrations of S100B (a marker of glial activation) and BDNF.
Neuroanatomically, the depression signature was characterized by GMV reductions primarily in limbic regions, such as the hippocampus and amygdala, which are central to emotion regulation and stress response. The presence of elevated BDNF alongside IL-4 (an anti-inflammatory cytokine) suggests a complex, potentially compensatory or dysregulated neuroplastic response in early-stage depression that is absent in the early stages of psychosis.
The Role of Childhood Trauma and Cognition
One of the most striking findings of the PRONIA study was the predictive power of psychosocial and cognitive features. Childhood trauma was a significant predictor for both the psychosis (balanced accuracy [BAC] = 67.2%) and depression (BAC = 78.0%) signatures. This suggests that early-life adversity may ‘program’ the neuro-immune system, leading to the specific brain-blood patterns observed in adulthood.
However, cognitive performance served as a diverging factor. While neurocognitive deficits were strong predictors of the psychosis signature (BAC = 65.1%), they did not significantly predict the depression signature. This indicates that while both disorders share a foundation in environmental stress, the neurobiological trajectory of psychosis is more closely linked to cognitive decline and corticothalamic dysfunction.
Expert Commentary: Challenging Dimensional Models
The findings of the PRONIA consortium provide a critical counterpoint to the prevailing view that mental disorders exist purely on a continuum. While symptoms like anhedonia or social withdrawal may overlap between depression and psychosis, the underlying brain-blood signatures appear distinct. This biological divergence suggests that a ‘one-size-fits-all’ approach to treating inflammation in psychiatry—such as using generic anti-inflammatory drugs—may be suboptimal. Instead, interventions may need to be tailored to the specific cytokine-neuroanatomical profile of the patient.
Furthermore, the study highlights the necessity of considering the ‘biological scars’ of childhood trauma. The high predictive accuracy of trauma history for these signatures reinforces the importance of trauma-informed care and suggests that early-life interventions could potentially mitigate the development of these neuro-immune signatures.
There are, however, limitations to consider. As a naturalistic study, although medication was minimal, it was not entirely absent for all participants. Additionally, the cross-sectional nature of the primary signatures requires further longitudinal validation to determine if these patterns can predict long-term outcomes or treatment responses.
Conclusion
The PRONIA study represents a significant step forward in the quest for biologically informed psychiatry. By identifying distinct neuro-immune signatures for early-stage depression and psychosis, the research provides a framework for moving beyond descriptive diagnosis toward mechanistic understanding. The integration of blood biomarkers, structural neuroimaging, and psychosocial history offers a multidimensional view of mental illness that could eventually guide targeted, early-stage interventions, potentially improving the trajectory for millions of patients worldwide.
Funding and Registration
The PRONIA study was supported by the European Union’s Seventh Framework Programme (FP7/2007-2013) under grant agreement n° 602452. Additional support was provided by various national funding bodies in the participating European countries. ClinicalTrials.gov Identifier: NCT01803542.
References
1. Popovic D, Weyer C, Dwyer DB, et al.; PRONIA Consortium. Multivariate Brain-Blood Signatures in Early-Stage Depression and Psychosis. JAMA Psychiatry. 2025 Dec 17:e253803. doi: 10.1001/jamapsychiatry.2025.3803. Epub ahead of print. PMID: 41405910; PMCID: PMC12712837.
2. Khandaker GM, Dantzer R. Is there a role for immune-to-brain communication in schizophrenia? Psychopharmacology (Berl). 2016;233(9):1559-1573.
3. Pariante CM. Why are the brain and the mind so inflamed? A 20-year journey from the lab bench to psychiatry. Psychol Med. 2017;47(12):2036-2052.