The Paradigm Shift in Pulmonary Embolism Management: Primary Results from STORM-PE
Acute pulmonary embolism (PE) remains the third leading cause of cardiovascular death worldwide. While therapeutic strategies for high-risk (massive) PE are well-established, the optimal management of intermediate-high risk (submassive) PE has long been a subject of clinical debate. These patients, characterized by hemodynamic stability but evidence of right ventricular (RV) strain and myocardial injury, face a significant risk of clinical deterioration. Historically, anticoagulation alone has been the standard of care, but concerns regarding its speed in relieving RV pressure overload have led to the exploration of advanced reperfusion therapies.
The STORM-PE trial (A Prospective, Multicenter, Randomized Controlled Trial Evaluating Anticoagulation Alone Versus Anticoagulation Plus Mechanical Aspiration With the Indigo Aspiration System for the Treatment of Intermediate-High Risk Acute Pulmonary Embolism) represents a landmark achievement in this space. It is the first randomized controlled trial (RCT) to evaluate the efficacy and safety of computer-assisted vacuum thrombectomy (CAVT) against the standard of anticoagulation alone.
Highlights
1. CAVT significantly outperformed anticoagulation alone in reducing the RV/LV diameter ratio at 48 hours, achieving a mean reduction of 0.52 compared to 0.24.
2. Patients treated with CAVT showed a markedly higher rate of vital sign normalization within the first 48 hours.
3. The trial demonstrated a significant reduction in pulmonary artery obstruction, as measured by refined modified Miller scores.
4. Major adverse event (MAE) rates within 7 days were statistically comparable between the two groups, supporting the safety profile of mechanical intervention.
The Clinical Dilemma of Intermediate-High Risk Pulmonary Embolism
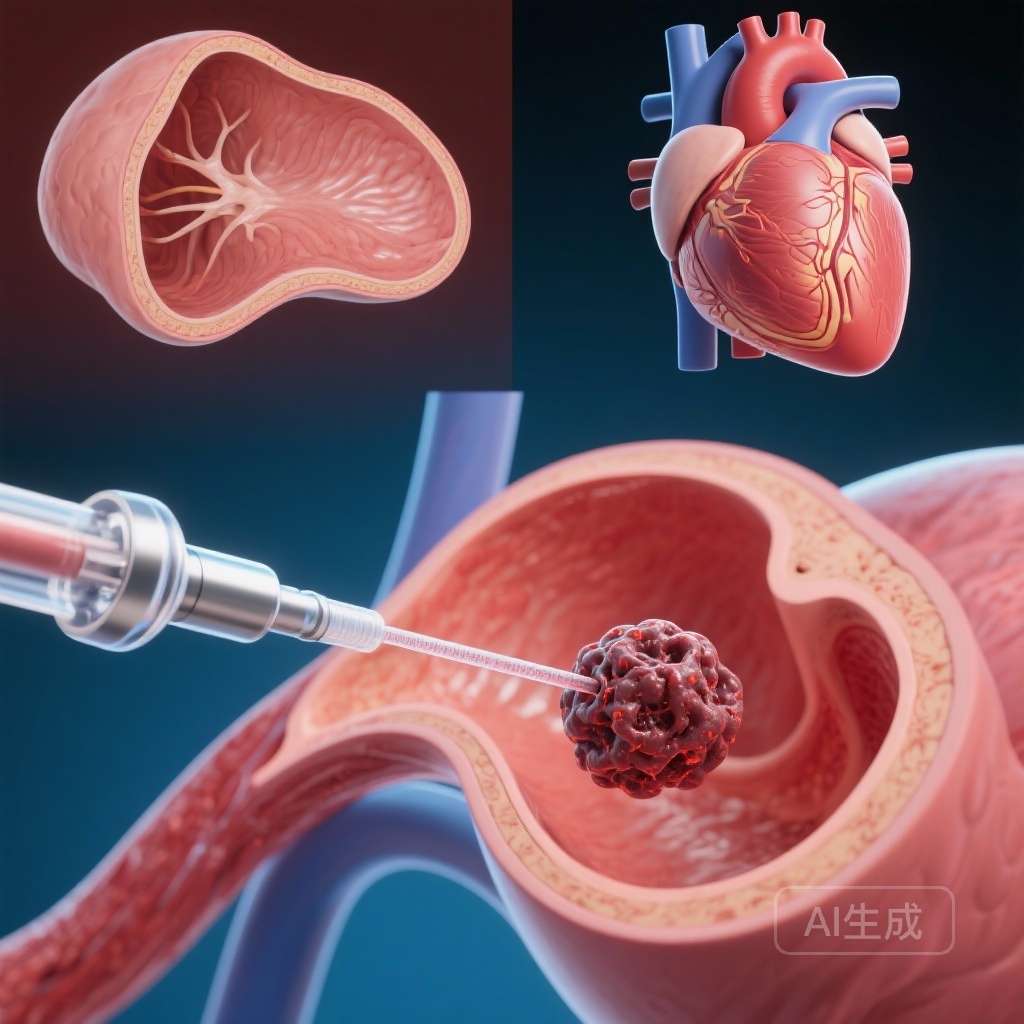
Intermediate-high risk PE is defined by the presence of both RV dysfunction (detected via imaging) and elevated cardiac biomarkers (such as troponin or BNP) in a patient who is currently normotensive. The primary clinical objective in these cases is to rapidly relieve acute RV pressure overload to prevent a downward spiral into hemodynamic collapse and obstructive shock. While systemic thrombolysis offers rapid reperfusion, it is associated with a high risk of major hemorrhage, particularly intracranial bleeding. Catheter-directed therapies, specifically CAVT, have emerged as a potentially safer alternative designed to physically remove the thrombus while minimizing systemic drug exposure and procedural blood loss.
STORM-PE Study Design: A Rigorous International RCT
STORM-PE was designed as an international, multicenter RCT with a 1:1 randomization protocol. The study enrolled 100 adult patients across 22 sites who presented with acute-onset PE symptoms (within 14 days). Inclusion criteria required patients to be normotensive but demonstrate an RV/LV ratio of ≥1.0 on computed tomographic pulmonary angiography (CTPA) alongside elevated cardiac biomarkers.
Patients were randomized to receive either CAVT using the Indigo Aspiration System (Penumbra, Inc.) in conjunction with anticoagulation, or anticoagulation alone. The Indigo system utilized in this trial features computer-assisted technology designed to optimize aspiration timing and reduce procedural blood loss by distinguishing between blood and clot. The primary endpoint was the change in the RV/LV ratio from baseline to 48 hours, assessed by an independent, blinded imaging core laboratory. Secondary endpoints included major adverse events (MAEs) within 7 days, changes in vital signs, and the degree of pulmonary artery obstruction.
Key Findings: Rapid Reversal of Right Ventricular Strain
The results of STORM-PE provide compelling evidence for the efficacy of CAVT. At the 48-hour mark, the mean reduction in the RV/LV ratio was 0.52 ± 0.37 in the CAVT group, compared to only 0.24 ± 0.40 in the anticoagulation-only group. This absolute difference of 0.27 (95% CI, 0.12–0.43; P < 0.001) highlights the superior ability of mechanical thrombectomy to rapidly unload the right ventricle.
Furthermore, the reduction in clot burden was significantly more pronounced in the CAVT arm. Both the modified Miller scores and refined modified Miller scores—validated metrics for pulmonary artery obstruction—showed significantly greater improvements in patients treated with CAVT (P < 0.001). Beyond imaging, the clinical impact was evident in the accelerated normalization of vital signs, suggesting that mechanical reperfusion leads to faster physiological stabilization than pharmacotherapy alone.
Safety Profile and Procedural Considerations
Safety is a paramount concern when introducing invasive interventions for stable patients. The STORM-PE trial reported that the MAE rate within 7 days was not significantly different between the groups (4.3% in the CAVT arm vs. 7.5% in the anticoagulation arm; P = 0.681). The MAE composite included clinical deterioration, PE-related mortality, recurrent PE, and major bleeding.
While two PE-related deaths occurred in the CAVT arm, the overall safety data suggests that the procedure does not inherently increase the risk of major complications compared to conservative management. The use of computer-assisted vacuum technology is particularly noteworthy here, as it addresses one of the historical limitations of mechanical thrombectomy: excessive blood loss. By utilizing sensors to modulate aspiration, the system allows for effective clot removal while preserving the patient’s hemoglobin levels.
Expert Commentary: Contextualizing STORM-PE
The STORM-PE trial marks a significant milestone in vascular medicine. Previous evidence for mechanical thrombectomy in PE was largely derived from single-arm prospective studies such as FLARE and EXTRACT-PE. While those studies demonstrated safety and efficacy, the lack of a randomized control group made it difficult to definitively conclude that thrombectomy was superior to anticoagulation alone. STORM-PE fills this critical gap in the literature.
From a clinical perspective, these findings suggest that for patients with significant RV strain, waiting for anticoagulation to naturally resolve the thrombus may be less efficient than active intervention. However, experts note that patient selection remains key. The trial specifically targeted “intermediate-high” risk patients, who are at the highest risk within the non-massive category. For lower-risk patients, the benefits of an invasive procedure may not outweigh the costs and procedural risks.
One limitation of the trial is the sample size of 100 patients, which, while sufficient for the primary endpoint, may not be powered to detect rare safety events or long-term outcomes such as the development of chronic thromboembolic pulmonary hypertension (CTEPH). Future research should focus on whether rapid RV recovery in the acute phase translates to improved functional capacity and quality of life in the long term.
Conclusion: A New Standard for Submassive PE?
The STORM-PE trial demonstrates that CAVT is superior to anticoagulation alone in achieving rapid RV decompression and reducing clot burden in intermediate-high risk PE patients. With a safety profile comparable to medical management and more rapid clinical stabilization, mechanical thrombectomy with CAVT is positioned to become a preferred strategy for patients with significant RV dysfunction. As the medical community moves toward a more proactive approach to PE, these results provide the evidence-based foundation needed to update clinical guidelines and refine treatment algorithms.
Funding and Clinical Registration
The STORM-PE trial was funded by Penumbra, Inc. The trial is registered at ClinicalTrials.gov with the unique identifier NCT05684796.
References
1. Lookstein RA, Konstantinides SV, Weinberg I, et al. Randomized Controlled Trial of Mechanical Thrombectomy With Anticoagulation Versus Anticoagulation Alone for Acute Intermediate-High Risk Pulmonary Embolism: Primary Outcomes From the STORM-PE Trial. Circulation. 2026;153(1):21-34.
2. Konstantinides SV, Meyer G, Becattini C, et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J. 2020;41(4):543-603.
3. Tu T, Toma C, Tapson VF, et al. A Therapeutic Aspiration Catheter for Pulmonary Embolism: May Treatment of the Acute Clot (EXTRACT-PE) Trial. JACC Cardiovasc Interv. 2019;12(16):1586-1596.