Introduction: The Unmet Need in Ischaemic Stroke Management
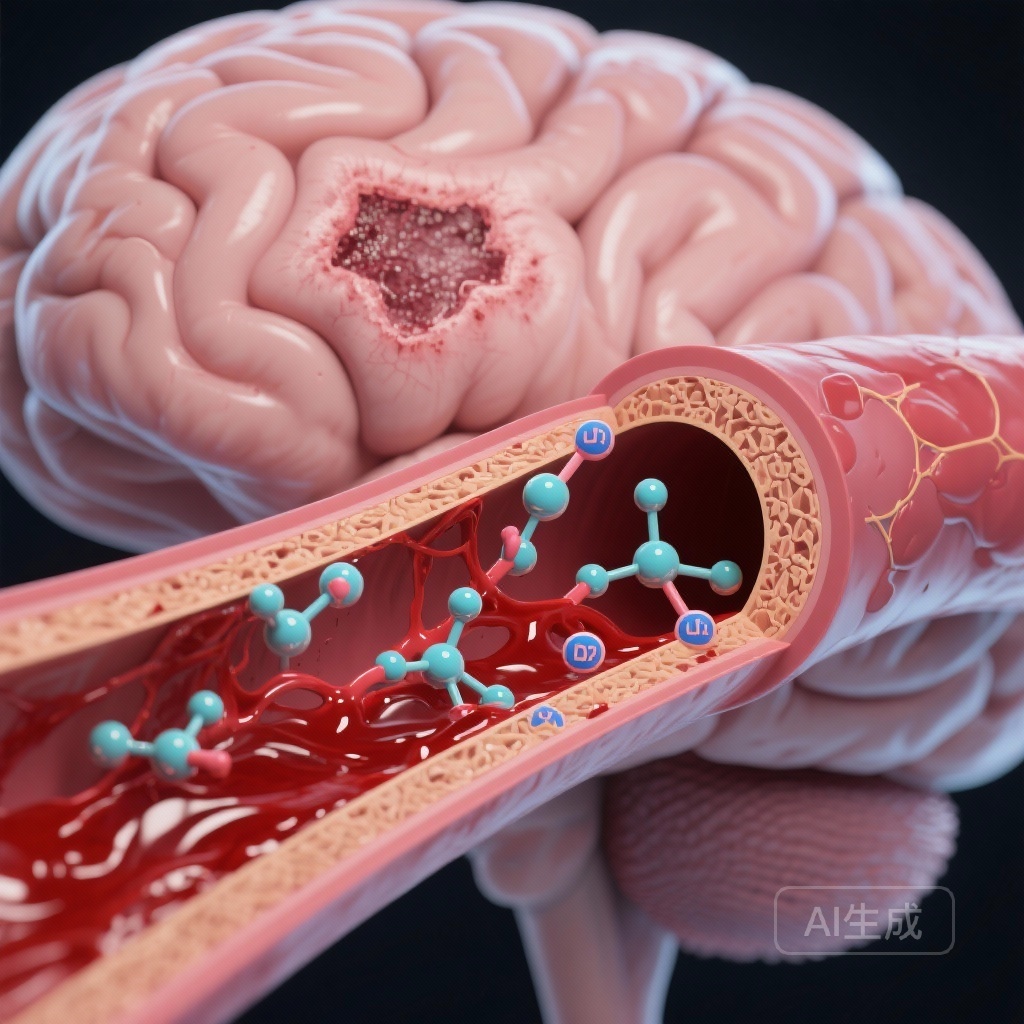
Ischaemic stroke remains a leading cause of global morbidity and mortality. Despite the revolutionary success of mechanical thrombectomy and intravenous thrombolysis, a significant proportion of patients continue to experience poor functional outcomes due to reperfusion injury, haemorrhagic transformation, and the progressive breakdown of the neurovascular unit. Current therapeutic strategies focus primarily on recanalisation, yet there is a critical lack of neuroprotective agents that can stabilize the blood-brain barrier (BBB) and prevent neuronal apoptosis in the aftermath of an acute event. Recent evidence published by Shi et al. in the European Heart Journal has shed light on a novel molecular player in this pathology: Dickkopf-related protein 2 (DKK2).
The Role of DKK2 in Neurovascular Pathophysiology
Dickkopf-related protein 2 is a known antagonist of the canonical Wnt/β-catenin signalling pathway, a pathway essential for vascular development, blood-brain barrier maintenance, and neuronal survival. While the role of Wnt signalling in central nervous system homeostasis is well-documented, the specific impact of its endogenous inhibitors, such as DKK2, in the context of acute cerebral ischaemia has remained poorly understood until now. The study by Shi and colleagues provides a comprehensive analysis of how DKK2 expression shifts during ischaemia and how this shift dictates the severity of brain injury.
Study Design and Methodology
The researchers employed a translational approach, combining animal models with clinical observational data. In the experimental arm, a murine model of transient middle cerebral artery occlusion (tMCAO) was used to simulate ischaemia and subsequent reperfusion. Genetic tools, including DKK2-knockout mice and viral-mediated overexpression, were utilized to establish causality. Furthermore, a monoclonal antibody (mAb) targeting DKK2 was tested to evaluate its therapeutic viability.
In the clinical arm, the study analysed DKK2 levels in the serum of stroke patients who had undergone endovascular treatment (EVT) for large vessel occlusion. This allowed the researchers to correlate circulating DKK2 levels with clinical parameters, including infarct volume, the occurrence of intracranial haemorrhage (ICH), and functional recovery as measured by the modified Rankin Scale (mRS) at 90 days.
Key Findings: From Bench to Bedside
Clinical Correlation in Stroke Patients
The clinical data revealed a striking correlation between DKK2 and stroke severity. Patients with higher baseline serum DKK2 levels following large vessel occlusion exhibited significantly larger infarct volumes. More importantly, elevated DKK2 was an independent predictor of haemorrhagic transformation, suggesting that the protein plays a role in compromising the structural integrity of cerebral microvessels. These findings suggest that serum DKK2 could serve as a potential biomarker for identifying patients at high risk of post-reperfusion complications.
Experimental Evidence of DKK2 Toxicity
In murine models, DKK2 expression was found to be significantly up-regulated in both the brain parenchyma and the systemic circulation following tMCAO. When DKK2 was overexpressed using viral vectors, the researchers observed a marked expansion of infarct size, worsened neurological deficits, and increased BBB permeability. Conversely, genetic deletion of DKK2 provided substantial neuroprotection, reducing infarct volume and preserving motor function.
Perhaps the most clinically relevant finding was the efficacy of the DKK2 monoclonal antibody. Systemic administration of the antibody significantly attenuated the deleterious effects of ischaemia, suggesting that DKK2 is accessible to pharmacological intervention and that its inhibition can salvage neurovascular function even after the onset of the stroke.
Mechanistic Insights: The RXRα-DKK2-Wnt Axis
To understand why DKK2 increases during ischaemia, the researchers investigated transcriptional regulation. They identified retinoid X receptor-alpha (RXRα) as a key upstream regulator. Under conditions of ischaemia/reperfusion, RXRα is activated in neurons, directly binding to the DKK2 promoter and driving its expression.
Once secreted, DKK2 acts in a paracrine and autocrine fashion to suppress canonical Wnt signalling. In the vasculature, this inhibition leads to the loss of tight junction proteins (such as Claudin-5 and ZO-1), resulting in BBB leakage. In neurons, the suppression of Wnt signalling triggers apoptotic pathways. By inhibiting DKK2, the researchers were able to restore Wnt/β-catenin activity, thereby stabilizing the neurovascular unit and promoting cell survival.
Expert Commentary: Translational Implications and Limitations
The identification of the RXRα-DKK2-Wnt axis represents a significant leap forward in our understanding of the ‘no-reflow’ phenomenon and reperfusion injury. For clinicians, the prospect of a monoclonal antibody that can be administered alongside standard reperfusion therapies is particularly exciting. Such a ‘cocktail’ approach—reopening the vessel while simultaneously blocking DKK2-mediated damage—could theoretically extend the therapeutic window and improve the safety profile of thrombolysis.
However, several questions remain. While the study demonstrates the efficacy of DKK2 inhibition in mice, the transition to human clinical trials requires careful consideration of timing and dosage. Additionally, because Wnt signalling is involved in many physiological processes, the long-term safety of systemic DKK2 inhibition must be thoroughly vetted. The observational nature of the human data also means that while DKK2 is a strong biomarker, more prospective studies are needed to confirm its predictive value across diverse patient populations.
Conclusion: A New Horizon for Stroke Therapy
Dickkopf-related protein 2 has emerged as a critical mediator of neurovascular dysfunction in ischaemic stroke. By elucidating the RXRα-DKK2-Wnt pathway, Shi et al. have provided a clear roadmap for the development of next-generation neuroprotective therapies. As we move toward a more personalized approach to stroke care, targeting DKK2 may offer a way to not only reduce brain damage but also to mitigate the devastating risks of haemorrhagic transformation, ultimately leading to better functional independence for patients.
References
1. Shi Z, Li J, Feng Z, et al. Dickkopf-related protein 2 impairs neurovascular Wnt signalling and worsens stroke outcome. Eur Heart J. 2025 Dec 26:ehaf959. doi: 10.1093/eurheartj/ehaf959.
2. Liebner S, Czupalla C, Wolburg H. Current concepts of blood-brain barrier development. Int J Dev Biol. 2011;55(4-5):467-76.
3. Nusse R, Clevers H. Wnt/β-Catenin Signaling, Disease, and Emerging Therapeutic Modalities. Cell. 2017;169(6):985-999.