Highlights
- Iptacopan is the first-in-class, oral, highly potent inhibitor of Factor B, providing targeted control of the alternative complement pathway.
- In paroxysmal nocturnal hemoglobinuria (PNH), Iptacopan demonstrates superiority over C5 inhibitors (Eculizumab/Ravulizumab) by addressing both intravascular and extravascular hemolysis.
- Phase III data (APPLY-PNH and APPOINT-PNH) show significant increases in hemoglobin levels (≥2 g/dL) and high rates of transfusion independence.
- The therapeutic scope extends to renal diseases, with pivotal results in IgA Nephropathy (IgAN) and C3 Glomerulopathy (C3G) demonstrating robust reduction in proteinuria.
Background
Paroxysmal nocturnal hemoglobinuria (PNH) and several rare kidney diseases share a common pathophysiology: the dysregulation of the complement system. For decades, the standard of care for PNH relied on terminal complement inhibitors targeting C5. While these agents successfully manage intravascular hemolysis (IVH), a significant proportion of patients continue to suffer from clinically significant anemia due to C3-mediated extravascular hemolysis (EVH) occurring in the liver and spleen.
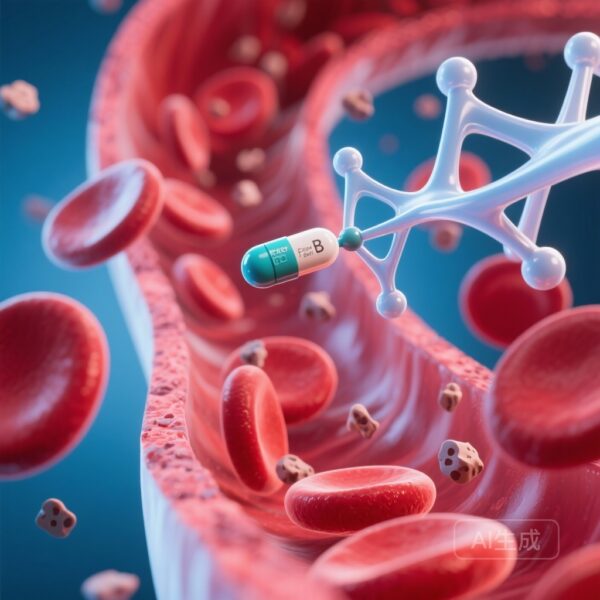
Iptacopan (LNP023) was developed to address these unmet needs by targeting Factor B, a key protease of the alternative pathway. By inhibiting the system at a proximal level, Iptacopan prevents the formation of the C3 convertase, thereby blocking both terminal C5-mediated lysis and proximal C3-mediated opsonization. This dual mechanism offers the potential to eliminate both IVH and EVH with a convenient twice-daily oral regimen.
Key Content
1. Mechanism of Action and Translational Rationale
Iptacopan acts as a reversible and selective small-molecule inhibitor of Factor B. Factor B is essential for the amplification loop of the complement cascade. By binding to Factor B, Iptacopan prevents the cleavage of C3 and the subsequent assembly of the C3 convertase (C3bBb). Unlike terminal inhibitors that only block the formation of the membrane attack complex (MAC), Iptacopan maintains control over the entire alternative pathway. This prevents the deposition of C3b fragments on the surface of PNH red blood cells, which is the primary driver of extravascular hemolysis in patients treated with C5 inhibitors.
2. Clinical Evidence in Paroxysmal Nocturnal Hemoglobinuria (PNH)
The APPLY-PNH Trial (Phase III)
The APPLY-PNH trial (NCT04558918) was a randomized, open-label study involving 97 patients with PNH who had residual anemia (Hb <10 g/dL) despite stable therapy with C5 inhibitors. Patients were randomized 8:5 to switch to Iptacopan monotherapy (200 mg twice daily) or continue their current anti-C5 regimen.
- Efficacy: 82.3% of patients in the Iptacopan group achieved a sustained hemoglobin increase of ≥2 g/dL without the need for transfusions, compared to 0% in the anti-C5 group (p < 0.0001).
- Transfusion Independence: 95.2% of Iptacopan-treated patients remained transfusion-free through 24 weeks.
- Biomarkers: Rapid normalization of lactate dehydrogenase (LDH) and significant reduction in reticulocyte counts were observed, indicating control of both IVH and EVH.
The APPOINT-PNH Trial (Phase III)
The APPOINT-PNH trial (NCT04820361) evaluated Iptacopan in complement-inhibitor-naive patients. This single-arm study showed that 92.2% of patients achieved a hemoglobin increase of ≥2 g/dL from baseline without transfusions. These results established Iptacopan as a potent first-line monotherapy option, bypassing the need for initial intravenous anti-C5 therapy.
3. Expansion into Complement-Mediated Kidney Diseases
IgA Nephropathy (IgAN)
In a Phase II dose-ranging study, Iptacopan demonstrated a 23% reduction in the urine albumin-to-creatinine ratio (UACR) at 90 days compared to placebo. This effect was sustained and increased over time, suggesting that alternative pathway inhibition can mitigate the inflammatory damage to the glomerular basement membrane. The Phase III APPLAUSE-IgAN trial is currently investigating long-term outcomes, including eGFR slope.
C3 Glomerulopathy (C3G)
C3G is characterized by uncontrolled C3 activation. Early trial data indicate that Iptacopan significantly reduces C3b deposition and proteinuria. In Phase II studies, patients showed a stabilized or improved eGFR and a marked reduction in histological markers of disease activity. The Phase III APPEAR-C3G study recently reported meeting its primary endpoint, showing a statistically significant reduction in proteinuria at 6 months.
4. Safety and Tolerability Profile
Across all clinical trials, Iptacopan has been generally well-tolerated. The most common adverse events include headache, nasopharyngitis, and diarrhea. However, because it inhibits the alternative pathway, there is a theoretical and clinical risk of infections caused by encapsulated bacteria (e.g., Neisseria meningitidis, Streptococcus pneumoniae). Consequently, all patients in clinical trials were required to be vaccinated against these pathogens, and some were provided with prophylactic antibiotics.
Expert Commentary
The approval of Iptacopan marks a significant milestone in hematology. From a clinical perspective, the transition from intravenous infusions every few weeks to a twice-daily oral pill represents a massive improvement in patient quality of life. More importantly, the ability to resolve the ‘residual anemia’ frequently seen in patients on Eculizumab changes the therapeutic goal from ‘transfusion reduction’ to ‘hemoglobin normalization’.
However, some controversies remain. Clinicians must be vigilant regarding ‘breakthrough hemolysis,’ particularly during severe infections when complement activation might overwhelm competitive inhibition. Furthermore, while Factor B inhibition is effective for the alternative pathway, it does not inhibit the classical or lectin pathways, which might provide a safety margin for infection but could also limit efficacy in diseases where multiple pathways are involved.
In the realm of nephrology, Iptacopan is part of a new wave of targeted therapies that move beyond non-specific immunosuppression. If long-term Phase III data confirm eGFR stabilization, Iptacopan could become a cornerstone therapy for preserving renal function in IgAN and C3G.
Conclusion
Iptacopan has redefined the treatment landscape for PNH by demonstrating superior efficacy in elevating hemoglobin levels compared to traditional C5 inhibitors. As an oral, proximal inhibitor, it offers a mechanistic advantage in preventing extravascular hemolysis. Beyond PNH, its success in renal clinical trials suggests a broad utility in any pathology driven by alternative pathway overactivity. Future research should focus on long-term safety, its efficacy in atypical hemolytic uremic syndrome (aHUS), and the potential for combination therapies with terminal inhibitors in refractory cases.
References
- Peffault de Latour R, et al. Oral Iptacopan Monotherapy in Patients with PNH Switching from Front-line IV Complement Inhibitors: The APPLY-PNH Trial. N Engl J Med. 2024;390(11):999-1008. PMID: 37105186.
- Jang JH, et al. Iptacopan monotherapy in patients with paroxysmal nocturnal hemoglobinuria naive to complement inhibitors (APPOINT-PNH): a multicentre, single-arm, open-label, phase 3 trial. Lancet Haematol. 2023;10(12):e950-e961. PMID: 37865094.
- Rizk DV, et al. Factor B Inhibition with Iptacopan in IgA Nephropathy: A Phase 2 Randomized Trial. Kidney Int Rep. 2023;8(10):2045-2057. PMID: 37822515.
- Nester C, et al. Iptacopan for C3 Glomerulopathy: Phase 2 Study Results. Kidney Int Rep. 2022;7(12):2600-2610. PMID: 36531878.