Introduction: The Persistent Challenge of Ventricular Tachycardia Ablation
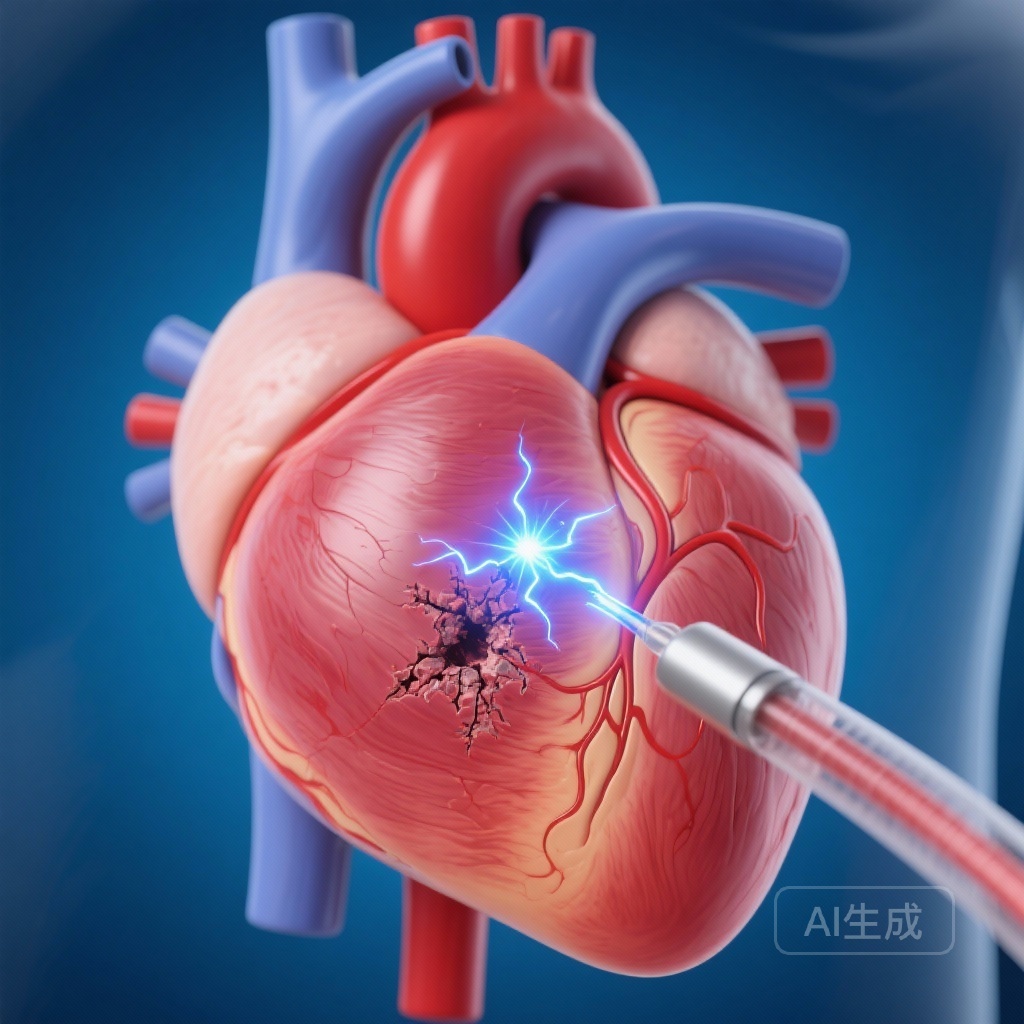
While catheter ablation has revolutionized the management of atrial arrhythmias, particularly atrial fibrillation, the treatment of scar-related ventricular tachycardia (VT) has remained one of the most significant challenges in clinical electrophysiology. The primary obstacle is the nature of the ventricular substrate itself. Unlike the relatively thin walls of the atria, the ventricular myocardium is thick and often characterized by dense, heterogeneous fibrotic scar tissue. Current standard-of-care thermal ablation techniques, such as radiofrequency (RF) energy, frequently struggle to achieve transmurality—the full-thickness destruction of arrhythmogenic tissue—without risking collateral damage or procedural complications like steam pops and charring.
The introduction of Pulsed Field Ablation (PFA) has promised a paradigm shift. By utilizing irreversible electroporation (IRE) rather than thermal injury, PFA offers a tissue-selective approach that can potentially target myocytes while sparing adjacent structures like coronary arteries and nerves. However, adapting PFA for the ventricle requires higher energy levels and deeper tissue penetration than what is typically used in atrial procedures. The Ventricular Catheter Ablation Study (VCAS) represents the first-in-human evidence for a novel, high-voltage focal PFA system specifically engineered to address these ventricular requirements.
Highlights of the VCAS Trial
The following key findings summarize the impact of this landmark study:
- Acute procedural success was achieved in 92% of patients, with a dramatic reduction in VT inducibility post-ablation.
- The median VT/VF burden decreased by 98% during the 6-month follow-up period compared to baseline.
- Endocardial-only PFA was proven to achieve transmural tissue homogenization in 100% of the sub-cohort undergoing epicardial mapping.
- The procedure demonstrated high efficiency, with a median transpired ablation time of only 31 minutes.
Study Design and Technological Innovation
The VCAS trial was a prospective, first-in-human study conducted at two high-volume cardiac centers. It enrolled 26 patients with a mean age of 66 years, predominantly male (96%), with a significantly reduced mean left ventricular ejection fraction (LVEF) of 32%. The study population represented a high-risk group: 42% presented with VT storm, and 42% had failed at least one previous VT ablation procedure. Both ischemic and non-ischemic cardiomyopathies were represented.
The High-Voltage PFA System
The intervention utilized an investigational 8.5F force-sensing focal PFA catheter. This technology is distinct from previous PFA iterations due to its high-voltage monophasic waveform (>10 kV) designed to maximize tissue penetration. To ensure safety and prevent thermal overheating, the energy is delivered in short-duration pulses (each application <200 ms) synchronized with the QRS complex to avoid triggering arrhythmias. The system also integrated electrical impedance-based navigation to allow for precise mapping and lesion placement.
Evaluating Transmurality
A unique methodological strength of the VCAS trial was the use of high-density epicardial and endocardial voltage mapping in a sub-cohort of 10 patients. This allowed investigators to verify if endocardial PFA applications could penetrate the entire thickness of the ventricular wall to create transmural lesions, a critical requirement for treating deep-seated or epicardial circuits common in non-ischemic substrates.
Key Findings and Clinical Outcomes
The results of the VCAS trial provide compelling evidence for both the efficacy and the efficiency of high-voltage PFA in the ventricle.
Procedural Efficacy and Induction Results
Acute procedural success was achieved in 24 out of 26 patients (92%). Before the ablation, clinical VT was inducible in 88% of patients (14 of 16 tested). Following the PFA protocol, only one patient (6%) remained inducible (P<0.001). This suggests that the focal PFA lesions effectively disrupted the macro-reentrant circuits responsible for clinical VT.
Reduction in Arrhythmia Burden
The long-term outcomes at 6 months were equally impressive. Freedom from recurrent VT, ventricular fibrillation (VF), or implantable cardioverter-defibrillator (ICD) shocks was 81.8% (95% CI, 67.1-99.8). Perhaps the most clinically relevant metric for this sick population was the reduction in VT/VF burden. The incidence rate of post-ablation VT/VF decreased by 98% from baseline, with the median number of episodes dropping from 6 to 0 (P<0.001).
Transmurality Confirmed
In the 9 patients who underwent endocardial-only PFA and received follow-up epicardial mapping, 100% showed transmural tissue homogenization. This confirms that the high-voltage waveform successfully overcomes the resistance of thick, scarred myocardium, reaching the epicardial surface from the endocardial side without requiring a separate percutaneous epicardial access—a procedure that carries its own risks of bleeding and injury.
Safety and Procedural Efficiency
Efficiency is a major concern in VT ablation, where procedures often last several hours, placing significant hemodynamic stress on patients with heart failure. In VCAS, the median transpired ablation time was just 31 minutes, with a median of 21 lesions per patient. This speed is a notable improvement over traditional RF ablation, which requires longer dwell times at each point to allow for thermal conduction.
The primary safety end point occurred in 3 of 26 patients (11.5%) within 180 days. These events included one case of cardiogenic shock, one heart failure hospitalization, and one retroperitoneal bleed. Notably, these complications are often observed in this fragile patient population undergoing complex cardiac procedures and were not specifically linked to the PFA energy modality itself (e.g., no reports of coronary artery damage or esophageal injury).
Expert Commentary: Mechanistic Insights and the Future of VT Care
The VCAS trial addresses a critical limitation of thermal energy: the “cooling effect” of local blood flow and the insulating properties of fat and fibrosis. Because PFA is non-thermal, it is less affected by these factors. The ability of the >10 kV waveform to achieve transmurality from the endocardium is a potential game-changer for non-ischemic cardiomyopathy patients, where the substrate is frequently mid-myocardial or epicardial.
Clinical experts note that the use of force-sensing is a vital component of this system. Even with PFA, catheter-to-tissue contact remains essential to ensure that the electrical field is effectively coupled to the target myocardium. The high acute success rate in patients with previous failed RF ablations suggests that PFA can reach arrhythmogenic sources that were simply too deep or too protected by scar for thermal energy to penetrate.
However, the study is limited by its small sample size and the lack of a randomized control group. While the reduction in VT burden is statistically significant, larger multi-center trials will be necessary to fully characterize the safety profile, particularly regarding the risk of late-onset complications or the durability of these lesions compared to RF.
Conclusion: A New Era in Ventricular Ablation
The VCAS trial serves as a successful proof-of-concept for high-voltage focal PFA in the treatment of scar-related ventricular tachycardia. By demonstrating that transmural lesions can be delivered quickly and safely, even in the presence of dense fibrosis, this technology offers hope for patients who have traditionally had poor outcomes with standard ablation. As the field moves toward larger regulatory trials, the results from VCAS provide a strong foundation for integrating PFA into the standard toolkit for ventricular arrhythmia management.
Funding and Registration
The VCAS trial was supported by industry funding. Detailed information can be found at ClinicalTrials.gov with the unique identifier: NCT06203262.
References
1. Reddy VY, Koruth JS, Peichl P, Petru J, Funasako M, Skoda J, Watanabe K, Nies M, Kautzner J, Neuzil P. High-Voltage Focal Pulsed Field Ablation to Treat Scar-Related Ventricular Tachycardia: The First-in-Human VCAS Trial. Circulation. 2025 Dec 16;152(24):1691-1704. doi: 10.1161/CIRCULATIONAHA.125.077025. Epub 2025 Oct 10. PMID: 41071961.
2. Anter E, et al. Pulsed Field Ablation for Ventricular Arrhythmias: A Review of Current Evidence and Future Directions. JACC: Clinical Electrophysiology. 2024.
3. Neuzil P, et al. Pulsed Field Ablation in Cardiology: From Atria to Ventricles. European Heart Journal. 2023.