Introduction: The Intersection of Nutrition and Environment in Early Atopy
The rising prevalence of atopic diseases, including atopic dermatitis, asthma, and allergic rhinitis, represents a significant global health burden. Atopic dermatitis (AD), often the first step in the so-called atopic march, frequently manifests in early infancy and significantly impacts the quality of life for both children and their families. While genetic predisposition is a known factor, the rapid increase in incidence suggests a critical role for environmental and nutritional modifiers during the prenatal and early postnatal periods. Among these, vitamin D has emerged as a key candidate for intervention due to its profound immunomodulatory effects. Recent evidence, however, suggests that the efficacy of vitamin D supplementation may not be uniform across the population but rather modified by environmental factors, most notably maternal tobacco exposure.
The COPSAC2010 Trial: High-Dose Supplementation and the Cotinine Modifier
A secondary analysis of the Copenhagen Prospective Studies on Asthma in Childhood 2010 (COPSAC2010) randomized clinical trial has provided groundbreaking insights into how maternal tobacco exposure influences the benefits of vitamin D. In this double-blinded study, 581 mother-child pairs were randomized to receive either a high dose of vitamin D3 (2800 IU/d) or a standard dose (400 IU/d) from the 24th week of pregnancy.
Study Methodology and Cotinine Profiling
To accurately assess tobacco exposure beyond self-reporting, researchers utilized maternal blood metabolomic profiling at the time of inclusion. A supervised sparse partial least squares model was employed to determine a maternal cotinine metabolome score, reflecting objective nicotine exposure. The primary outcomes tracked were the development of atopic dermatitis, asthma, and allergic rhinitis through the age of 6 years.
Key Results: A Personalized Prevention Signal
The findings revealed a significant effect modification by the maternal cotinine metabolome. High-dose vitamin D supplementation was particularly effective in reducing the risk of atopic dermatitis in the offspring of mothers with the highest tobacco exposure (fourth quartile). In this specific subgroup, the crude hazard ratio (HR) for AD was 0.46 (95% CI, 0.23-0.93, P = .03). When adjusted for potential confounders—including sex, birth season, socioeconomic status, air pollution, and maternal diet—the protective effect became even more pronounced, with an adjusted HR of 0.36 (95% CI, 0.15-0.85, P = .02). A similar effect modification was observed regarding the risk of asthma (P-interaction = .03), although the trend for allergic rhinitis did not reach statistical significance (P-interaction = .08).
The EDEN Birth Cohort: Cord Blood Vitamin D as a Predictive Marker
Complementing the COPSAC findings, the Etude des Déterminants pré et post natals du développement et de la santé de l’Enfant (EDEN) birth cohort examined the relationship between vitamin D levels at the time of birth and subsequent allergic outcomes. While the COPSAC study focused on the intervention dose, the EDEN study focused on the biological status of the neonate through cord serum 25-hydroxyvitamin D (25[OH]D) levels.
Findings on Wheezing and Atopic Dermatitis
In a cohort of 239 newborns followed for five years, the median cord serum 25(OH)D level was 17.8 ng/mL. Using multivariable-adjusted logistic regression, the researchers identified a significant inverse association between cord vitamin D levels and the risk of transient early wheezing and atopic dermatitis. Specifically, higher levels of 25(OH)D at birth were associated with a reduced risk of both early-onset and late-onset atopic dermatitis by ages 1, 2, 3, and 5 years. Interestingly, like the COPSAC study, no significant association was found between cord serum vitamin D and the development of allergic rhinitis or asthma by age 5.
Mechanistic Insights: The Tobacco-Vitamin D Interaction
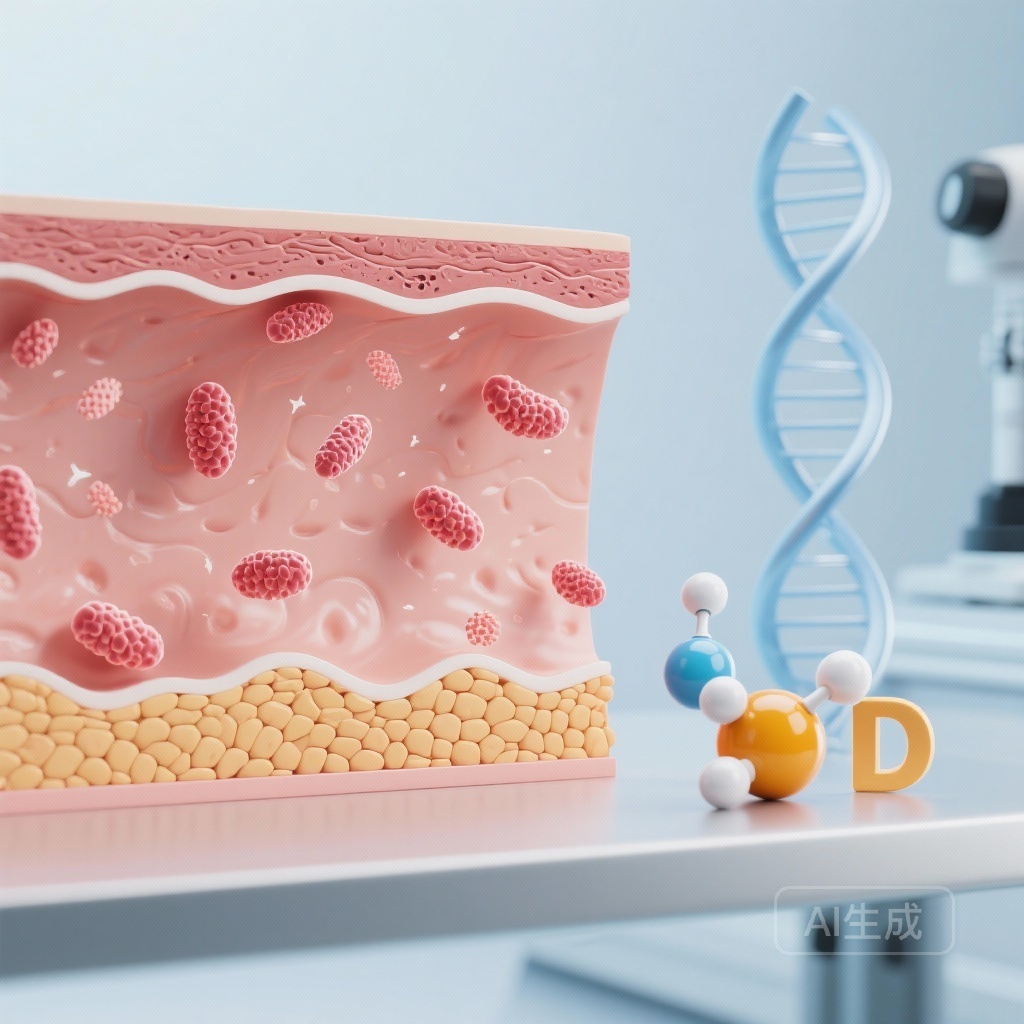
The biological plausibility of tobacco exposure modifying vitamin D efficacy is rooted in the complex interplay between environmental toxins and nutrient metabolism. Tobacco smoke contains polycyclic aromatic hydrocarbons and other chemicals that can induce oxidative stress and alter the expression of enzymes involved in vitamin D metabolism, such as CYP24A1 and CYP27B1.
Immune Maturation and Epigenetic Modification
Vitamin D is essential for the induction of regulatory T cells and the maintenance of the skin barrier. Tobacco exposure is known to skew the immune system toward a Th2-mediated allergic response. It is hypothesized that in the presence of high tobacco exposure, the developing immune system is under greater stress, making the anti-inflammatory and barrier-stabilizing effects of high-dose vitamin D more clinically impactful. Furthermore, tobacco and vitamin D may have opposing epigenetic effects on genes related to lung development and immune signaling, suggesting that high-dose supplementation may counteract some of the deleterious epigenetic modifications induced by smoking.
Clinical Implications for Prenatal Care
These studies suggest that the current standard recommendation for prenatal vitamin D (often 400-600 IU/d) may be insufficient for certain subgroups, particularly those exposed to environmental tobacco smoke.
The Case for Personalized Supplementation
The COPSAC2010 data supports a personalized approach to prenatal nutrition. For mothers with high tobacco exposure—whether through active smoking or significant secondhand exposure—high-dose vitamin D (2800 IU/d) may serve as a crucial primary preventive measure against childhood atopic dermatitis and asthma. Clinicians should consider screening for tobacco exposure more rigorously, perhaps utilizing biomarkers like cotinine, to identify those who would benefit most from higher vitamin D doses.
Limitations and Future Directions
While these findings are compelling, they are not without limitations. The COPSAC2010 analysis was a post hoc secondary analysis, and the EDEN study featured a relatively small sample size. Furthermore, the exploratory nature of the cotinine metabolome score requires validation in larger, diverse cohorts. Future research should investigate whether these findings extend to other environmental pollutants and whether the timing of supplementation earlier in pregnancy provides even greater benefits.
Conclusion
The evidence from these two distinct cohorts highlights a critical window of opportunity in the prenatal period. Vitamin D is not merely a bone-health nutrient but a potent modifier of the early immune landscape. The discovery that its protective effects against atopy are most pronounced in the context of tobacco exposure offers a pathway toward precision medicine in maternal-fetal health. By targeting high-dose vitamin D to mothers with environmental risk factors, we may significantly reduce the incidence of the atopic march in the next generation.
Funding and Clinical Trials
The COPSAC2010 trial is registered at ClinicalTrials.gov (NCT00856947). The study was supported by various independent research grants and public health funds.
References
1. Brustad N, Wang T, Chen L, et al. Effect of prenatal high-dose vitamin D on childhood atopic dermatitis is modified by maternal cotinine metabolome: A secondary analysis of a randomized clinical trial. J Am Acad Dermatol. 2026;94(1):88-95. doi:10.1016/j.jaad.2025.08.044.
2. Baïz N, Dargent-Molina P, Wark JD, et al. Cord serum 25-hydroxyvitamin D and risk of early childhood transient wheezing and atopic dermatitis. J Allergy Clin Immunol. 2014;133(1):147-53. doi:10.1016/j.jaci.2013.05.017.