Introduction: The Rationale for GSK-3β Inhibition in Refractory Malignancies
Glycogen synthase kinase 3β (GSK-3β) has emerged as a multifaceted therapeutic target in oncology. Unlike many kinases that function primarily as oncogenes, GSK-3β plays a complex role, regulating pathways involved in cell cycle progression, epithelial-mesenchymal transition (EMT), and the maintenance of cancer stem cells. In several aggressive malignancies, including salivary gland carcinoma (SGC) and pancreatic ductal adenocarcinoma (PDAC), aberrant nuclear localization of GSK-3β (nGSK-3β) has been identified as a driver of therapeutic resistance and tumor progression.
Elraglusib (9-ING-41) is a potent, small-molecule inhibitor of GSK-3β designed to overcome these resistance mechanisms and potentially enhance the efficacy of conventional chemotherapy and immunotherapy. Two recent Phase II clinical trials have investigated the safety and efficacy of elraglusib in these challenging clinical settings, providing critical insights into its role in precision oncology.
Study 1: Elraglusib in Recurrent and Metastatic Salivary Gland Carcinoma
Salivary gland carcinomas represent a heterogeneous group of rare tumors. Among them, adenoid cystic carcinoma (ACC) is known for its indolent but relentless progression and limited sensitivity to systemic therapies. In a Phase II, open-label trial led by Hanna et al., researchers evaluated elraglusib in combination with chemotherapy, with or without immunotherapy priming, for patients with recurrent or metastatic SGC.
Study Design and Patient Population
The trial enrolled 32 patients, stratified into two main histological groups: ACC (47%) and non-ACC (53%). The study utilized two cohorts to explore different therapeutic combinations:
1. Cohort 1: Elraglusib (15 mg/kg) plus platinum-based chemotherapy (carboplatin or cisplatin).
2. Cohort 2: Pembrolizumab (immunotherapy) priming for two cycles followed by the elraglusib/chemotherapy regimen.
The primary endpoint was the best overall response rate (ORR) according to RECIST v1.1 criteria.
Clinical Outcomes and the Biomarker Significance of nGSK-3β
The trial did not meet its primary endpoint, recording an overall ORR of 9.4% (3 out of 32 patients). All three partial responses occurred in the non-ACC subgroup. Despite the low ORR, 59% of patients achieved stable disease, leading to a median progression-free survival (PFS) of 6.4 months and a median overall survival (OS) of 18.6 months.
A pivotal finding of this study was the correlation between nuclear GSK-3β expression and treatment response. Responders exhibited a median nGSK-3β expression of 50%, compared to only 2% in non-responders. This suggests that nGSK-3β may serve as a critical predictive biomarker for identifying patients most likely to benefit from elraglusib therapy.
Safety and Tolerability
The safety profile was consistent with expected toxicities of platinum-based regimens, though elraglusib added specific considerations. Common adverse events included anemia (69%), nausea (50%), and neutropenia (44%). The investigators noted that while the primary endpoint was not reached for the entire population, the 18% response rate in the non-ACC cohort receiving immune priming warrants further investigation in specific histological subtypes.
Study 2: Elraglusib Combined with Gemcitabine and Nab-Paclitaxel in Metastatic Pancreatic Cancer
Pancreatic ductal adenocarcinoma (PDAC) remains one of the most lethal cancers, characterized by a dense stroma and significant chemoresistance. Given that GSK-3β is known to promote the survival of pancreatic cancer cells under metabolic stress, the combination of elraglusib with the standard-of-care regimen (Gemcitabine/Nab-paclitaxel, GnP) was evaluated in a Phase II study by Mahalingam et al.
Trial Methodology
This nonrandomized, Simon’s two-stage study enrolled 42 patients with previously untreated metastatic PDAC. Patients received elraglusib at an initial dose of 15 mg/kg twice weekly in combination with standard GnP. The primary endpoint was the disease control rate (DCR).
Efficacy Results
The study reported a DCR of 35.7% and an ORR of 26.2%. The median PFS was 5.4 months, and the median OS was 11.9 months. While these results show preliminary clinical activity, they also highlighted the challenges of combining novel kinase inhibitors with intensive cytotoxic backbones in a fragile patient population.
Dose-Limiting Toxicities and Visual Impairment
The safety analysis revealed significant treatment-emergent adverse events (TEAEs). Grade 3 or higher TEAEs occurred in 85.7% of patients, including neutropenia (52.4%) and fatigue (21.4%). Notably, 83.3% of patients experienced visual impairment, a side effect specifically associated with elraglusib in this combination.
Due to the exacerbation of GnP-related toxicities and frequent dose interruptions, the protocol was amended to reduce the elraglusib dose to 9.3 mg/kg. This dose reduction was found to be better tolerated and is currently being evaluated in a randomized Phase II study to determine if the efficacy can be maintained while mitigating high-grade toxicities.
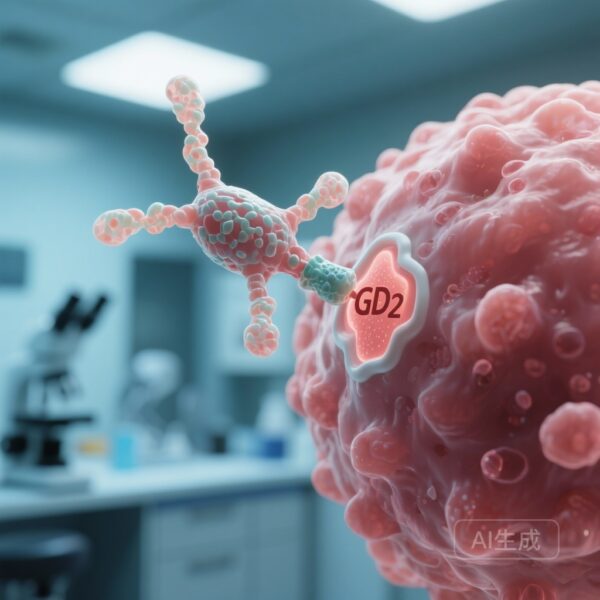
Mechanistic Insights: Why Nuclear Localization Matters
The divergent results in these trials underscore a fundamental biological principle of GSK-3β: its function is highly dependent on its subcellular localization. In many cells, cytoplasmic GSK-3β acts as a negative regulator of the Wnt/β-catenin pathway. However, when GSK-3β moves into the nucleus, it can stabilize pro-survival transcription factors like NF-κB and c-Myc, promoting tumor growth and resistance to apoptosis.
The findings in the salivary gland trial—where responders had significantly higher nuclear GSK-3β—validate this mechanism. It suggests that elraglusib’s primary value may not be as a broad-spectrum inhibitor, but as a precision tool for tumors that have specifically co-opted nuclear GSK-3β signaling.
Expert Commentary and Clinical Implications
The clinical development of elraglusib represents an important step in targeting the “non-oncogene addiction” of cancer cells to stress-response kinases. While neither trial demonstrated a transformative breakthrough for all-comer populations, they provided a clear roadmap for future research:
1. Biomarker-Driven Selection: Future trials in SGC should prioritize patients with high nGSK-3β expression, potentially focusing on non-ACC subtypes where activity was more pronounced.
2. Rational Combinations: The pancreatic cancer trial suggests that while GSK-3β inhibition can complement chemotherapy, the therapeutic window is narrow. Managing off-target effects like visual impairment is crucial for maintaining patient quality of life and treatment adherence.
3. Immunotherapy Synergy: The potential for elraglusib to prime the immune microenvironment, as seen in the SGC trial, remains an area of high interest, particularly in “cold” tumors like PDAC and ACC.
Conclusion
Elraglusib shows modest but identifiable clinical activity in advanced salivary gland and pancreatic cancers. The Phase II data emphasize that the path forward for GSK-3β inhibitors lies in precision medicine. By utilizing nuclear GSK-3β expression as a selection criterion and optimizing dosing schedules to manage toxicity, elraglusib may yet find a role in the multi-modal management of refractory solid tumors.
Funding and Clinical Trial Registry
The salivary gland carcinoma trial was supported by Actuate Therapeutics and registered at ClinicalTrials.gov (NCT04218071). The pancreatic cancer study was also supported by Actuate Therapeutics and registered at ClinicalTrials.gov (NCT03678883).
References
1. Hanna GJ, Scarfo N, Shin KY, et al. Elraglusib, a Glycogen Synthase Kinase 3β Inhibitor, plus Chemotherapy with or without Immunotherapy in Patients with Recurrent, Metastatic Salivary Gland Carcinoma. Clin Cancer Res. 2026;32(1):83-93.
2. Mahalingam D, Saeed A, Powell SF, et al. Phase II study of elraglusib (9-ING-41), a GSK-3β inhibitor, in combination with gemcitabine plus nab-paclitaxel in previously untreated metastatic pancreatic cancer. ESMO Open. 2025;10(6):105122.