Introduction
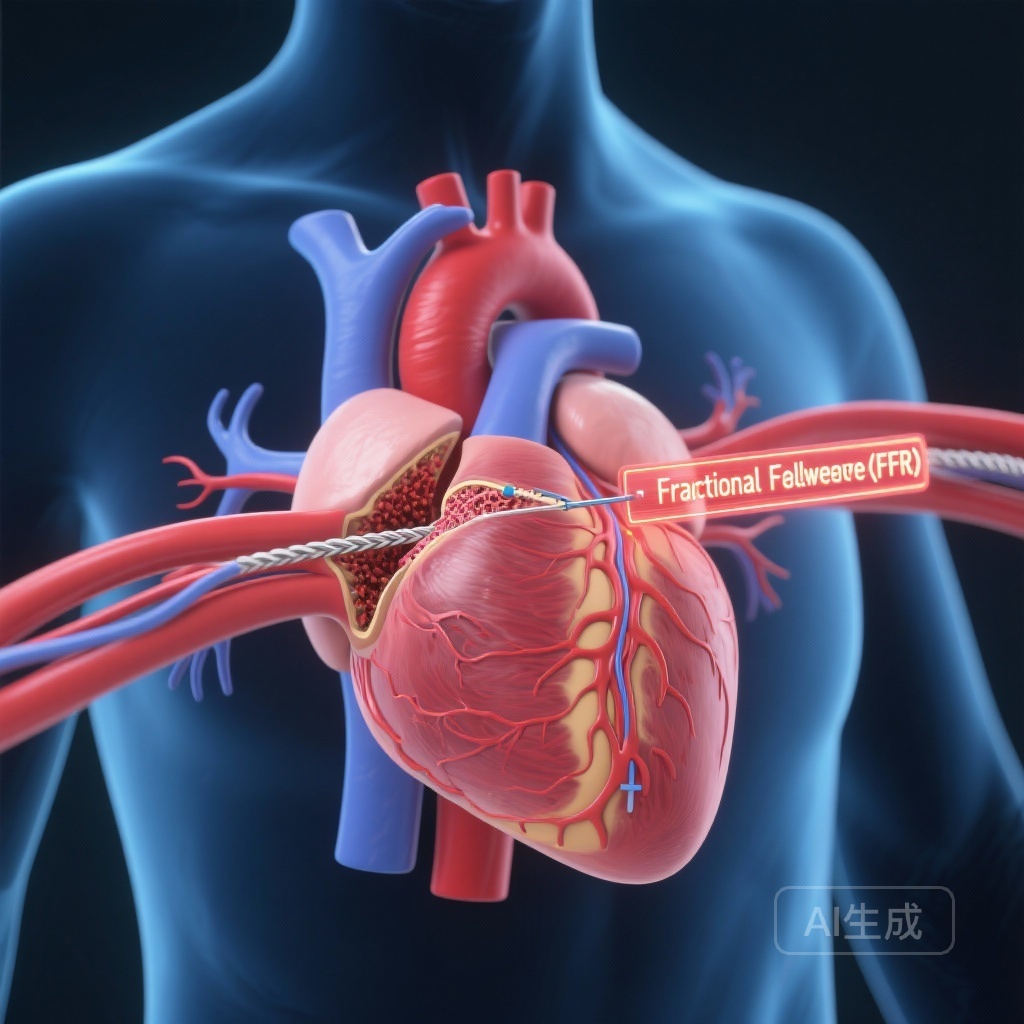
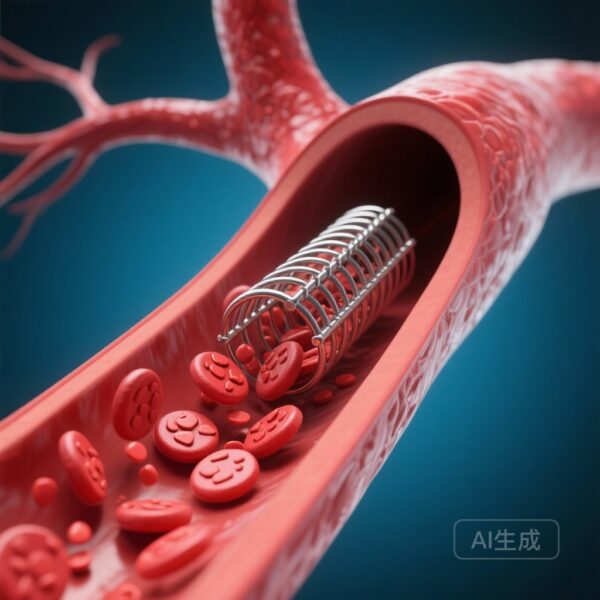
The clinical management of patients presenting with both severe aortic stenosis (AS) and concomitant coronary artery disease (CAD) remains one of the most debated topics in interventional cardiology. As transcatheter aortic valve replacement (TAVR) has expanded into younger and lower-risk populations, the long-term impact of untreated coronary lesions has come to the forefront of clinical concern. Historically, the decision to perform percutaneous coronary intervention (PCI) in TAVR candidates was guided primarily by visual angiographic assessment, which is known to be a poor predictor of the physiological significance of a lesion. While Fractional Flow Reserve (FFR) is the gold standard for guiding revascularization in stable CAD, its validity in the presence of severe AS has been questioned due to potential alterations in hyperemic flow. The NOTION-3 (Nordic Aortic Valve Intervention-3) trial provides much-needed evidence on whether an FFR-guided strategy can optimize outcomes for this complex patient cohort.
Background and Clinical Context
Approximately 40% to 50% of patients undergoing TAVR have significant CAD. The presence of CAD is associated with worse outcomes, yet unnecessary PCI carries risks of vascular complications, bleeding from dual antiplatelet therapy, and contrast-induced nephropathy. Current guidelines have provided weak recommendations regarding the timing and necessity of PCI in TAVR patients, often relying on expert consensus rather than robust randomized data. The primary physiological concern with using FFR in these patients is that the high left ventricular end-diastolic pressure and microvascular changes associated with severe AS might blunt the maximal hyperemic response, potentially leading to false-negative FFR results (values >0.80 despite significant obstruction). The NOTION-3 trial was designed to address these uncertainties by evaluating the prognostic value of FFR in assessing coronary stenosis before TAVR.
Study Design and Methodology
The NOTION-3 trial was a multicenter study that enrolled patients from a randomized trial and a prospective registry. The study included patients with severe aortic stenosis scheduled for TAVR who also had at least one coronary artery stenosis of 50% or greater by visual assessment.
Patient Stratification
A total of 587 patients were analyzed. The cohort was divided based on FFR values and treatment assignment:1. FFR ≤0.80 Conservative Group (n=232): Patients with significant ischemia-producing lesions who were managed conservatively.2. FFR ≤0.80 PCI Group (n=220): Patients with significant lesions (or stenosis ≥90%) who underwent percutaneous coronary intervention.3. FFR >0.80 Defer Group (n=135): Patients whose FFR values were above the ischemic threshold and had their revascularization deferred.
Endpoints
The primary composite outcome was the incidence of cardiovascular death, myocardial infarction (MI), and/or urgent revascularization through 36 months of follow-up. A lesion-level analysis was also performed to evaluate the safety of deferring treatment based on FFR.
Key Findings and Results
The results of NOTION-3 provide a compelling argument for the use of FFR in the TAVR workup. The study found significant differences in the cumulative incidence of the primary composite endpoint over the 3-year follow-up period.
Primary Composite Outcomes
The cumulative incidence rates for cardiovascular death, MI, or urgent revascularization were:21.6% in the FFR ≤0.80 conservative group.11.5% in the FFR ≤0.80 PCI group.10.5% in the FFR >0.80 defer group.The difference between the groups reached statistical significance (P = 0.003). Crucially, the risk in the FFR ≤0.80 conservative group was roughly double that of the other two groups. The excess risk observed in the conservative group was primarily driven by significantly higher rates of myocardial infarction and the need for urgent revascularization.
Lesion-Level Analysis
When examining outcomes at the level of individual coronary segments, the data further supported the physiological approach. Revascularization was required in 12.6% of conservatively treated segments with an FFR ≤0.80. In contrast, only 1.3% of segments treated with PCI and 0.9% of segments where treatment was deferred based on an FFR >0.80 required subsequent intervention (P < 0.0001).
Consistency of the 0.80 Threshold
One of the most important takeaways from the trial is that patients with FFR >0.80 (the Defer group) had outcomes nearly identical to those who received PCI for significant lesions (10.5% vs 11.5%). This suggests that the standard 0.80 threshold remains a reliable indicator of clinical safety even in the hemodynamic environment of severe aortic stenosis.
Expert Commentary and Clinical Implications
The NOTION-3 trial represents a milestone in the movement toward physiology-guided intervention in the TAVR population. For years, clinicians have struggled with whether to treat moderate coronary lesions discovered during TAVR workup.
Addressing the Hyperemia Controversy
The fear that severe AS would make FFR unreliable appears to be largely mitigated by these findings. If FFR were truly blunted by AS, we would have expected the ‘Defer’ group (FFR >0.80) to show a higher rate of late events as those ‘missed’ lesions became symptomatic after the valve was replaced. However, the low event rate in the deferral group (10.5%) confirms that FFR is a robust gatekeeper for PCI in this setting.
Practical Application
Based on NOTION-3, a clear clinical pathway emerges: for TAVR candidates with coronary stenosis between 50% and 90%, FFR should be utilized. If the FFR is ≤0.80, revascularization provides a clear benefit in reducing long-term MI and urgent revascularization. If the FFR is >0.80, PCI can be safely deferred, sparing the patient from the risks of an unnecessary procedure.
Limitations
While the study is robust, it is important to note that it focused on stable CAD. The management of acute coronary syndromes in TAVR candidates remains a separate clinical challenge. Additionally, the study utilized a 3-year follow-up; longer-term data will be essential as TAVR continues to move into younger populations with longer life expectancies.
Conclusion
The NOTION-3 trial clarifies the role of FFR in the TAVR population, demonstrating that a conservative approach to physiologically significant coronary lesions (FFR ≤0.80) is associated with a doubling of cardiovascular risk compared to PCI. Furthermore, the study confirms that deferring treatment for lesions with FFR >0.80 is safe and leads to outcomes comparable to successful revascularization. These findings support the routine integration of FFR into the pre-TAVR diagnostic workup to ensure that revascularization is targeted to those patients who will derive the greatest prognostic benefit.
Funding and Trial Information
The NOTION-3 trial was supported by various academic and clinical research grants. ClinicalTrials.gov Identifier: NCT03058627.
References
1. Jørgensen TH, et al. Fractional Flow Reserve to Guide Revascularization in Patients With Coronary Artery Disease Undergoing TAVR. JACC Cardiovasc Interv. 2025 Dec 8;18(23):2925-2936. doi: 10.1016/j.jcin.2025.10.015. PMID: 41371788.
2. Tonino PA, et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med. 2009;360(3):213-224.
3. Fearon WF, et al. Fractional Flow Reserve-Guided PCI as Compared with Coronary-Artery Bypass Graft Surgery. N Engl J Med. 2022;386(2):128-137.