Highlights
– In the Dallas Heart Study-2 cohort (n = 3,401), higher electromechanical activation time (EMAT) measured by acoustic cardiography was independently associated with lower left ventricular ejection fraction (LVEF) and larger LV volumes.
– EMAT had poor discrimination for reduced LVEF (C-statistic 0.52), performed worse than NT‑proBNP (C = 0.59), and did not improve discrimination beyond NT‑proBNP.
– Although baseline EMAT predicted cardiovascular death/heart failure hospitalization and major adverse clinical events in minimally adjusted models, associations were no longer significant after adjustment for NT‑proBNP.
Background
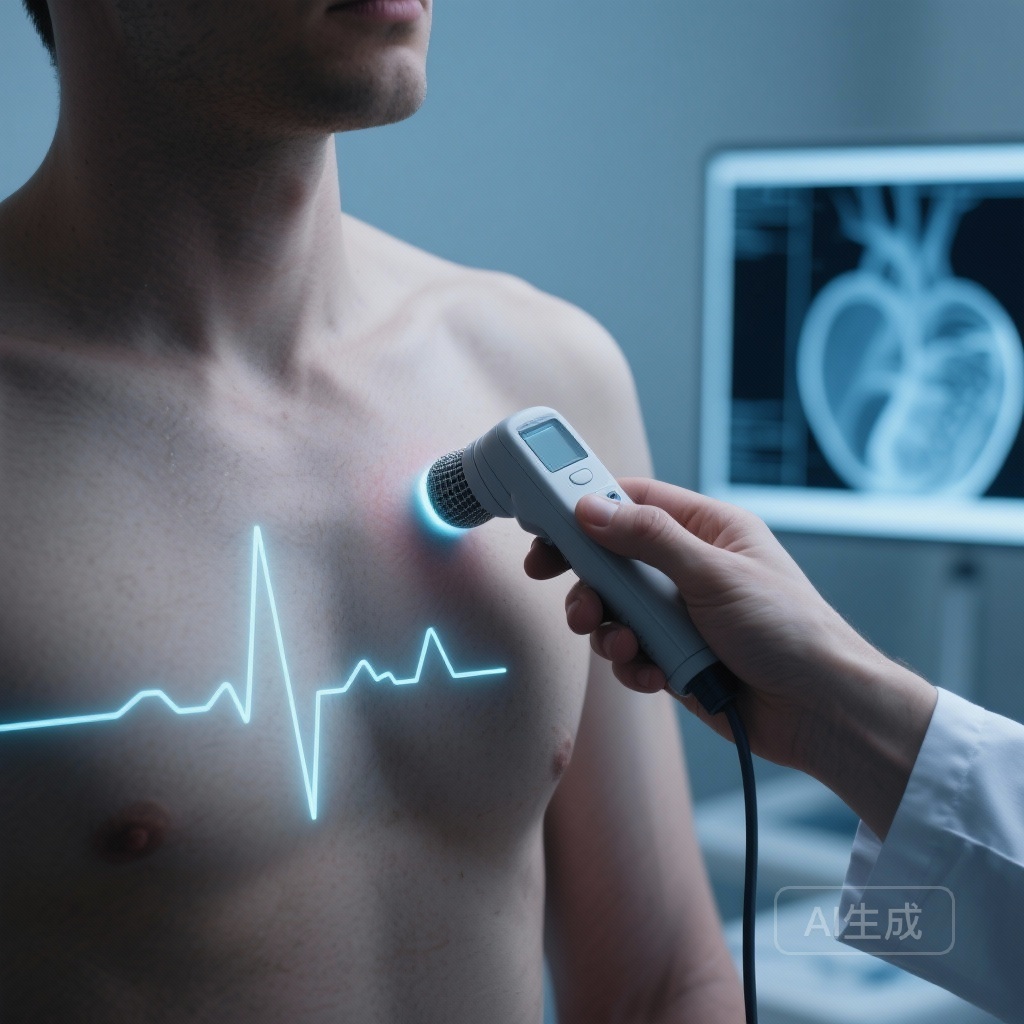
Detecting left ventricular systolic dysfunction and identifying individuals at elevated risk for heart failure (HF) are central goals of community cardiovascular screening. Natriuretic peptides, particularly N-terminal pro-B-type natriuretic peptide (NT‑proBNP), are well established as biomarkers for diagnosing and prognosticating HF and for risk stratification in community populations. Acoustic cardiography is a noninvasive technique that combines phonocardiography with electrocardiography to quantify electromechanical aspects of cardiac function. Electromechanical activation time (EMAT), the interval from QRS onset to the first heart sound, is hypothesized to reflect the delay between electrical depolarization and the onset of effective mechanical systole and has been associated with systolic dysfunction in prior small studies.
Study design
This analysis used baseline data from Dallas Heart Study-2, a multiethnic, population-based cohort. A total of 3,401 participants underwent acoustic cardiography (yielding EMAT), cardiac magnetic resonance imaging (CMR) for precise measurement of cardiac structure and function, and blood sampling including NT‑proBNP measurement. Participants were followed for clinical outcomes over a median of 12.4 years. Prespecified outcomes included a composite of cardiovascular (CV) death or HF hospitalization and a broader major adverse clinical events (MACE) endpoint comprising CV death, HF hospitalization, nonfatal myocardial infarction, stroke, and atrial fibrillation.
Analytic methods included multivariable regression to examine associations between continuous EMAT and CMR-derived measures (LVEF, LV volumes) and Cox proportional hazards models for outcomes. Models adjusted sequentially for demographics (age, sex, race) and then for established biomarkers including NT‑proBNP. Discrimination for reduced LVEF (<55% per CMR) was assessed using C-statistics and compared between EMAT and NT‑proBNP and with combined models.
Key findings
Baseline associations with cardiac structure and function
Higher continuous EMAT was independently associated with lower LVEF (P < 0.001) and with greater left ventricular end-diastolic volume (P = 0.04) after multivariable adjustment for demographic and clinical covariates. These associations are consistent with the physiologic premise that prolonged electromechanical delay accompanies impaired systolic performance and ventricular remodeling.
Discrimination for reduced LVEF
Despite statistically significant associations, EMAT demonstrated poor discrimination for reduced LVEF when evaluated as a screening test. The C-statistic for EMAT to detect LVEF <55% was 0.52, essentially equivalent to chance. By comparison, NT‑proBNP had modest discrimination (C = 0.59), which was statistically superior to EMAT (P < 0.01). Adding EMAT to NT‑proBNP did not improve discrimination beyond NT‑proBNP alone (P = 0.90).
Prognostic associations
In models adjusted for age, sex, and race, baseline EMAT was associated with the composite of CV death and HF hospitalization (hazard ratio [HR] 1.3 per unit increase; 95% CI: 1.2–1.4; P < 0.001) and with the broader MACE endpoint (HR 1.2; 95% CI: 1.1–1.4; P < 0.001). However, when NT‑proBNP was included in the models, these associations were attenuated and no longer significant (P > 0.10), indicating that NT‑proBNP captured the prognostic information associated with EMAT.
Net clinical value
The data indicate that while EMAT correlates with structural and functional cardiac abnormalities and with adverse outcomes in minimally adjusted models, it neither discriminates reduced LVEF effectively nor adds incremental prognostic information to NT‑proBNP in a community-dwelling population.
Expert commentary and interpretation
Physiologic plausibility and prior literature: The electromechanical interval measured by EMAT reflects the time between electrical activation and the mechanical first heart sound (closure of the mitral valve associated with onset of ventricular systole). In systolic dysfunction, impaired contractility and altered loading conditions can prolong the interval, consistent with the observed association between EMAT and lower LVEF.
Performance as a screening biomarker: Performance characteristics of a screening test must include discrimination, calibration, practicality, and incremental value over existing tools. Although EMAT is noninvasive and can be obtained rapidly with acoustic cardiography devices, its poor discrimination for reduced LVEF (C = 0.52) limits its utility as a stand-alone screening tool in the general population. The modestly superior discrimination of NT‑proBNP and the absence of incremental value when both markers are combined suggest that NT‑proBNP remains the preferred biomarker for community screening and risk stratification.
Possible niches for EMAT: The device-based nature of EMAT measurement may be attractive in low-resource settings where point-of-care biomarker testing is limited, but poor discrimination cautions against reliance on EMAT alone. EMAT could have niche applications in remote or bedside monitoring where repeated measures and trends (rather than single thresholds) are informative; however, this remains speculative and requires prospective evaluation.
Limitations and generalizability
The Dallas Heart Study-2 is a valuable multiethnic cohort, but generalizability beyond the sampled population depends on differences in comorbidity burden, prevalence of structural heart disease, and device standardization. Acoustic cardiography measurements can be influenced by signal quality, body habitus, and operator technique; reproducibility and standardized thresholds for EMAT were not established as part of the community screening context. The study used CMR-derived LVEF as the reference standard, which strengthens internal validity but does not alter the fundamental finding that EMAT lacks discriminative power for reduced LVEF at the population level.
Clinical implications
For clinicians and health systems considering expanded screening strategies for asymptomatic LV systolic dysfunction, these results counsel against adopting EMAT as a primary screening tool. NT‑proBNP retains greater discriminative ability and encompasses the prognostic signal that EMAT provides. From a practical standpoint, if acoustic cardiography devices are already in use in a clinical program, EMAT may provide supplementary physiologic information, but it should not replace natriuretic peptide testing or imaging when the goal is accurate detection of reduced LVEF or risk prediction.
Recommendations for future research
Future studies should explore whether serial EMAT measurements (trajectory over time) have incremental prognostic value beyond single time-point assessments and NT‑proBNP. Comparative effectiveness research examining cost, accessibility, and combined multimodal screening algorithms (symptom questionnaires, biomarkers, device-derived indices) may clarify pragmatic roles for acoustic cardiography. Standardization of EMAT acquisition and prespecified thresholds aligned with clinical decision-making would be essential preconditions for implementation trials.
Conclusion
In this large, community-based cohort with long-term follow-up, prolonged EMAT measured by acoustic cardiography correlated with adverse cardiac structure and function and with worse clinical outcomes in minimally adjusted models. However, EMAT provided poor discrimination for reduced LVEF and did not add independent prognostic information beyond NT‑proBNP. These findings indicate that, while physiologically informative, EMAT is unlikely to displace or augment NT‑proBNP as a community screening biomarker for systolic dysfunction without further evidence from targeted implementation or serial-measurement studies.
Funding and clinicaltrials.gov
The original study citation lists funding sources and institutional support as reported by the authors; readers should consult the primary publication for detailed disclosures and sponsor roles. ClinicalTrials.gov registration details for Dallas Heart Study components can be found through the study’s institutional pages.
References
1) Munch J, Ayers CR, Grodin JL, Thibodeau JT, Hendren NS, Araj FG, Hardin EA, de Lemos JA, Shah AM, Pandey A, Drazner MH. Associations of Electromechanical Activation Time With Cardiac Structure and Function and Clinical Outcomes. JACC: Advances. 2025 Nov 27;5(1):102371. doi: 10.1016/j.jacadv.2025.102371. Epub ahead of print. PMID: 41313906.
2) Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. European Heart Journal. 2016;37(27):2129–2200. doi:10.1093/eurheartj/ehw128.