Highlight
– In TARGET‑FIRST (N=1,942 randomized), early discontinuation of aspirin after 1 month of uneventful DAPT in low‑risk acute MI patients was noninferior to continuing DAPT for the composite of death, MI, stent thrombosis, stroke, or major bleeding at 11 months.
– P2Y12‑inhibitor monotherapy reduced clinically relevant bleeding (BARC 2, 3, or 5) from 5.6% to 2.6% (HR 0.46; 95% CI, 0.29–0.75; P=0.002) without an increase in stent thrombosis or serious adverse events.
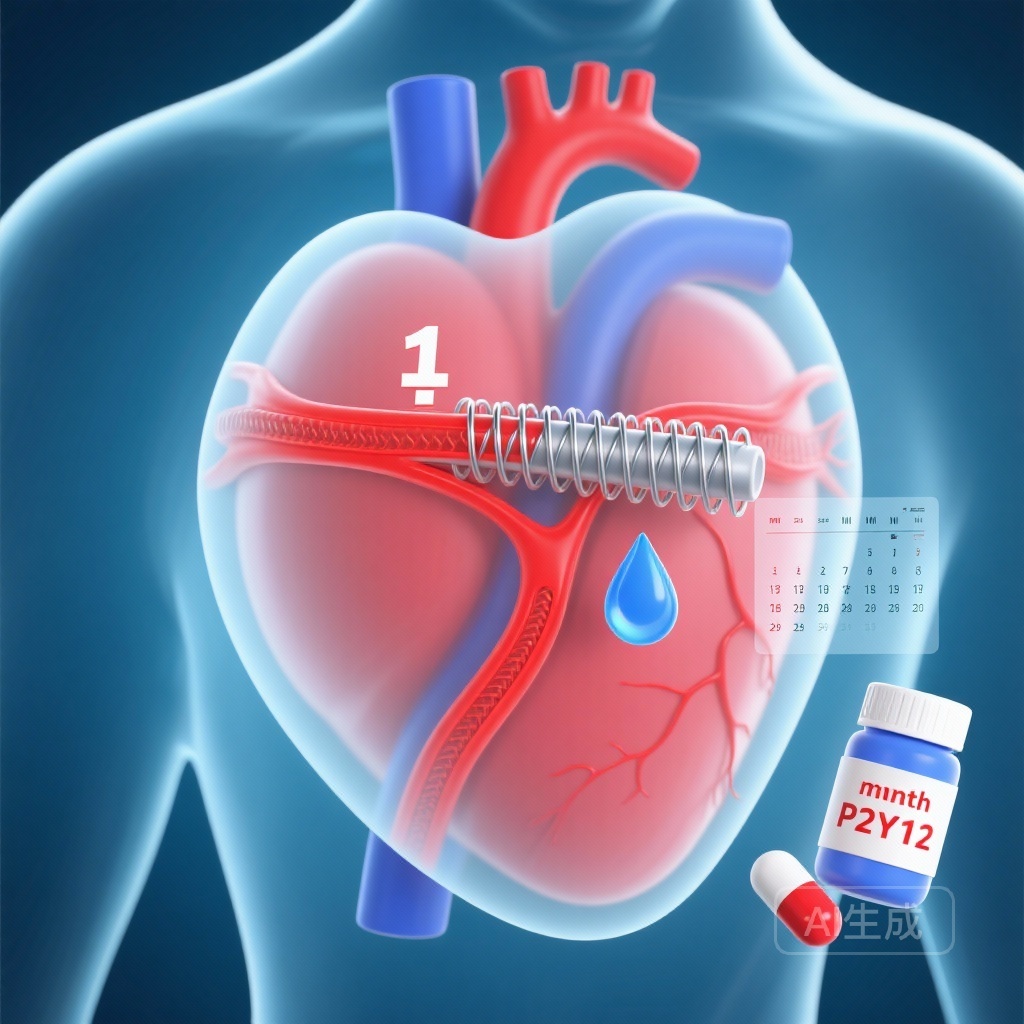
Background
Dual antiplatelet therapy (DAPT), typically aspirin plus a P2Y12 inhibitor, is foundational after percutaneous coronary intervention (PCI) to limit ischemic complications such as stent thrombosis and recurrent myocardial infarction. However, prolonged DAPT increases bleeding risk, which is independently associated with morbidity and mortality. Contemporary practice has shifted with newer-generation drug‑eluting stents, improved procedural techniques, and routine use of P2Y12 inhibitors with greater potency. These advances have prompted reevaluation of the optimal duration and composition of antiplatelet therapy, especially for patients with acute myocardial infarction (MI) who have undergone complete revascularization and who tolerate early therapy well.
Study design
The TARGET‑FIRST trial was a multicenter, open‑label, randomized study conducted at 40 European sites. Key eligibility criteria included adult patients with acute myocardial infarction who underwent successful complete revascularization within 7 days of the index MI, and who had completed 1 month of DAPT without ischemic or major bleeding events. After this run‑in, patients were randomized to either:
- Transition to P2Y12‑inhibitor monotherapy (aspirin discontinued) for the subsequent 11 months; or
- Continue dual antiplatelet therapy (aspirin plus P2Y12 inhibitor) for the additional 11 months.
The primary endpoint was a composite of death from any cause, myocardial infarction, stent thrombosis, stroke, or major bleeding defined as Bleeding Academic Research Consortium (BARC) type 3 or 5 at 11 months after randomization. Noninferiority was tested using an absolute margin of 1.25 percentage points. The main secondary endpoint was clinically relevant bleeding, defined as BARC type 2, 3, or 5, tested for superiority.
Key findings
Study population and randomization: Of 2,246 enrolled patients, 1,942 passed the 1‑month run‑in without major events and were randomized—961 to P2Y12‑inhibitor monotherapy and 981 to continued DAPT. Baseline characteristics reflected a low‑risk cohort: patients had early, guideline‑recommended complete revascularization and no ischemic or major bleeding events in the first month.
Primary outcome
The composite primary outcome occurred in 20 patients (2.1%) assigned to P2Y12‑inhibitor monotherapy and 21 patients (2.2%) assigned to continued DAPT. The absolute difference was −0.09 percentage points (95% CI, −1.39 to 1.20), meeting the prespecified noninferiority criterion (P = 0.02 for noninferiority). Thus, stopping aspirin after 1 month did not result in a higher rate of the composite ischemic/major bleeding endpoint compared with continuing DAPT.
Bleeding outcomes (main secondary)
Clinically relevant bleeding (BARC 2, 3, or 5) occurred in 2.6% of patients in the P2Y12‑inhibitor monotherapy arm versus 5.6% in the DAPT arm. This represented a hazard ratio of 0.46 (95% CI, 0.29–0.75; P = 0.002), indicating a 54% relative reduction in clinically relevant bleeding with aspirin discontinuation.
Ischemic safety
Stent thrombosis events were infrequent and similar between groups. Rates of death, recurrent MI, and stroke did not differ meaningfully, and the incidence of serious adverse events appeared comparable across arms. There was no signal that early aspirin withdrawal increased ischemic risk in this selected low‑risk population.
Interpretation of effect sizes
The absolute reduction in clinically relevant bleeding (approximately 3 percentage points) is clinically meaningful, particularly given the known adverse consequences of bleeding. The very low event rates for the composite ischemic/major bleeding outcome reflect careful patient selection (complete revascularization, uneventful first month) and contemporary PCI practice.
Expert commentary and clinical context
TARGET‑FIRST contributes to a growing body of evidence evaluating P2Y12‑inhibitor monotherapy after abbreviated DAPT. The trial’s strengths include its randomized design, pragmatic enrollment across multiple European centers, and clinically relevant endpoints (including standardized BARC bleeding definitions). The finding that aspirin can be stopped after 1 month without excess ischemic events in selected low‑risk MI patients is consistent with the hypothesis that, in contemporary practice, potent P2Y12 inhibition may provide the majority of antiplatelet protection after PCI while avoiding aspirin‑associated bleeding.
Several considerations are important when placing these results in practice:
- Patient selection: TARGET‑FIRST enrolled low‑risk patients who completed 1 month of DAPT uneventfully and had early complete revascularization. Extrapolation to higher‑risk patients (complex multivessel disease not fully revascularized, prior stent thrombosis, active malignancy, high ischemic burden) is not supported by these data.
- Choice of P2Y12 inhibitor: The trial allowed contemporary P2Y12 agents; the balance of ischemic protection and bleeding risk may differ between clopidogrel, ticagrelor, and prasugrel, particularly in populations with variable clopidogrel responsiveness.
- Open‑label design: Knowledge of treatment assignment could influence management or event reporting, although objective endpoints (death, MI, stent thrombosis) are less vulnerable to bias.
- Event rates and power: The low absolute rates of ischemic events increase uncertainty around rare events (e.g., stent thrombosis). Noninferiority margins and confidence intervals should be interpreted in light of absolute risks.
Biological plausibility and mechanism
Aspirin irreversibly inhibits platelet cyclooxygenase‑1, reducing thromboxane A2 production, but also predisposes to gastrointestinal and other bleeding. P2Y12 inhibitors block ADP‑mediated platelet aggregation and, when potent agents are used, provide substantial antithrombotic activity that may be sufficient to prevent stent‑related thrombosis. The combination of early stent endothelialization with potent monotherapy may explain why aspirin can be safely removed in selected patients after a brief period of dual therapy.
Limitations and unanswered questions
- Generalisability: The trial population was low risk—results cannot be extrapolated to high‑ischemic or high‑bleeding risk patients, to those with incomplete revascularization, or to patients with periprocedural complications.
- Heterogeneity of P2Y12 agents: The relative performance of specific P2Y12 inhibitors (clopidogrel vs ticagrelor vs prasugrel) as monotherapy was not the focus and requires further study.
- Long‑term outcomes: The follow‑up period was 11 months after randomization; longer‑term ischemic and bleeding outcomes deserve evaluation.
- Subgroup data and PCI complexity: Detailed subgroup analyses by stent length, number, bifurcation intervention, or presence of diabetes will be necessary to refine selection criteria.
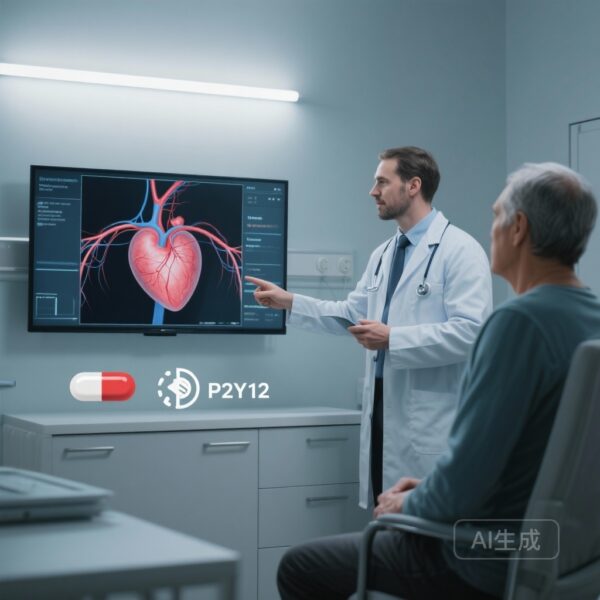
Clinical implications and practical recommendations
For clinicians caring for patients with acute MI who undergo successful early complete revascularization and who complete 1 month of DAPT without ischemic or major bleeding complications, TARGET‑FIRST supports consideration of stopping aspirin and continuing P2Y12‑inhibitor monotherapy for the remainder of the year. Key practical points:
- Carefully assess patient eligibility—this strategy is best applied to patients matching the trial entry profile (low risk, complete revascularization, uneventful first month).
- Choose a P2Y12 inhibitor thoughtfully. When clopidogrel is used, consider variability in antiplatelet response; potent P2Y12 inhibitors may offer greater ischemic protection but have different bleeding profiles and cost/side‑effect considerations.
- Shared decision‑making: discuss with patients the tradeoff between modestly lower ischemic risk of prolonged DAPT versus bleeding risk; for many patients, reduced bleeding may meaningfully improve quality of life and reduce hospitalizations.
- Monitor closely during the early post‑randomization months for any signs of ischemia or bleeding and reassess therapy if clinical circumstances change.
Research implications and future directions
Further research is needed to:
- Define which P2Y12 inhibitor is optimal for monotherapy in different patient subgroups.
- Identify biomarkers or platelet function tests that predict safety of aspirin withdrawal.
- Assess applicability in higher‑risk cohorts (e.g., complex PCI, left main disease, incomplete revascularization) and in diverse global populations.
- Evaluate longer‑term outcomes beyond 12 months and cost‑effectiveness of abbreviated DAPT with P2Y12 monotherapy.
Conclusion
In the TARGET‑FIRST randomized trial of low‑risk acute MI patients with early complete revascularization and an uneventful first month of DAPT, stopping aspirin and continuing P2Y12‑inhibitor monotherapy was noninferior for a composite of ischemic and major bleeding outcomes and produced a clinically important reduction in bleeding. These data support a patient‑selective strategy of early aspirin discontinuation after PCI, balancing ischemic risk, bleeding risk, and patient preferences. Wider adoption should be guided by careful patient selection and further confirmatory data in broader and higher‑risk populations.
Funding and trial registration
The trial was funded by MicroPort (France). TARGET‑FIRST ClinicalTrials.gov number: NCT04753749.
References
1. Tarantini G, Honton B, Paradies V, Lemesle G, Range G, Godin M, Mangin L, Cuisset T, Ruiz‑Nodar JM, Brugaletta S, Lhermusier T, Piot C, De Poli F, Macia JC, Motreff P, Madera‑Cambero M, Beygui F, Riccini P, Ranc S, Oreglia JA, Vaquerizo B, Poezevara Y, Bouchez D, Smits PC, Cayla G; TARGET‑FIRST Investigators. Early Discontinuation of Aspirin after PCI in Low‑Risk Acute Myocardial Infarction. N Engl J Med. 2025 Nov 27;393(21):2083-2094. doi: 10.1056/NEJMoa2508808. Epub 2025 Aug 31. PMID: 40888726.
Note: Additional trials and guideline statements have explored shortened DAPT durations and P2Y12‑inhibitor monotherapy strategies; clinicians should interpret TARGET‑FIRST within the totality of evidence and current guideline recommendations when applying the findings to individual patients.