Highlight
The Phase 2b IMPACT trial provides critical insights into the evolving landscape of Metabolic Dysfunction-Associated Steatohepatitis (MASH) pharmacotherapy. Key highlights include:
- Significant MASH Resolution: Both 1.2 mg and 1.8 mg doses of pemvidutide achieved MASH resolution without worsening of fibrosis in over 50% of patients at 24 weeks, compared to 20% in the placebo group.
- No Dose Titration Required: Unlike many GLP-1-based therapies, pemvidutide was administered without a titration period, showing a favorable tolerability profile with minimal discontinuations due to adverse events.
- Temporal Dynamics of Fibrosis: While MASH resolution was rapid, fibrosis improvement did not reach statistical significance at the 24-week mark, highlighting the potential need for longer-term intervention to observe structural liver remodeling.
Background: The Evolution of MASH Therapeutics
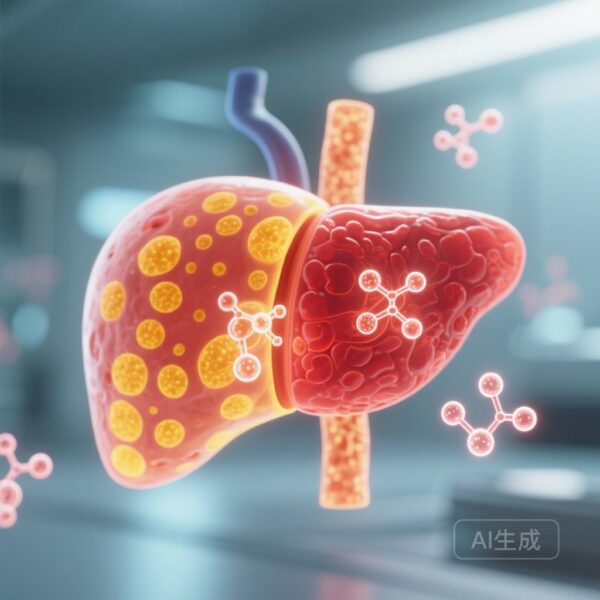
Metabolic dysfunction-associated steatohepatitis (MASH) remains a significant global health burden, characterized by hepatic steatosis, inflammation, and progressive fibrosis. For years, the therapeutic landscape was marked by limited options, but the recent emergence of incretin-based therapies has shifted the paradigm. While Glucagon-Like Peptide-1 (GLP-1) receptor agonists have demonstrated efficacy in weight loss and glycemic control, their direct impact on hepatic pathology is often considered secondary to weight reduction.
Pemvidutide represents a next-generation approach: a dual agonist of both GLP-1 and glucagon receptors. While GLP-1 reduces appetite and improves insulin sensitivity, the addition of glucagon receptor agonism is hypothesized to directly increase hepatic energy expenditure and promote lipid oxidation. This dual mechanism aims to target the liver more aggressively, potentially accelerating the clearance of hepatic fat and the resolution of inflammation compared to GLP-1 mono-agonists.
Study Design: The IMPACT Trial Methodology
The IMPACT trial was designed as an international, multicenter, randomised, double-blind, placebo-controlled, phase 2b study. The inclusion criteria focused on a high-risk population: patients with biopsy-confirmed MASH and liver fibrosis at stages F2 or F3 (moderate to advanced fibrosis). A total of 212 patients from 83 sites across the USA and Australia were enrolled.
Participants were randomly assigned in a 1:2:2 ratio to receive once-weekly subcutaneous injections of either placebo, 1.2 mg pemvidutide, or 1.8 mg pemvidutide. Notably, the study utilized a fixed-dose regimen without the standard dose titration often required for GLP-1 agonists to mitigate gastrointestinal side effects. The dual primary endpoints were assessed via liver biopsy at 24 weeks: MASH resolution without worsening of fibrosis, and at least a one-stage improvement in liver fibrosis without worsening of MASH.
Key Findings: Histological and Metabolic Efficacy
The 24-week results of the IMPACT trial offer a robust signal for the efficacy of dual agonism in resolving hepatic inflammation.
MASH Resolution
Pemvidutide demonstrated a clear, statistically significant advantage in achieving MASH resolution. In the 1.2 mg group, 58% of patients (24 of 41) achieved resolution (difference of 38% vs. placebo; p<0.0001). In the 1.8 mg group, 52% (45 of 85) achieved resolution (difference of 32% vs. placebo; p<0.0001). In contrast, only 20% of the placebo group (18 of 86) showed resolution. These data suggest that the dual mechanism of pemvidutide acts rapidly to clear the histological hallmarks of steatohepatitis.
Fibrosis Improvement
Regarding the second primary endpoint—fibrosis improvement of at least one stage without worsening of MASH—the results were less definitive at this interim timepoint. Fibrosis improvement was observed in 33% of the 1.2 mg group and 36% of the 1.8 mg group, compared to 28% in the placebo group. The differences (5% and 8% respectively) did not reach statistical significance (p=0.59 and p=0.27). This suggests that while inflammatory processes respond quickly to pemvidutide, the regression of established collagen deposits in the liver may require a longer duration of treatment than 24 weeks.
Safety and Tolerability
The safety profile of pemvidutide was a critical secondary outcome, especially given the lack of dose titration. Adverse events (AEs) were reported in 78% of the 1.2 mg group and 81% of the 1.8 mg group, compared to 67% in the placebo group. The majority of these events were gastrointestinal in nature and classified as mild or moderate. Discontinuation rates due to AEs were remarkably low: 0% in the 1.2 mg group and only 1% in the 1.8 mg group, compared to 2% in the placebo group. This suggests that the molecule is well-tolerated even at therapeutic doses from the start of treatment.
Expert Commentary: Mechanistic Insights and Clinical Implications
The results of the IMPACT trial underscore the biological plausibility of the GLP-1/glucagon dual agonist approach. In MASH, the liver is overwhelmed by lipid influx and impaired lipid handling. Glucagon agonism is known to stimulate mitochondrial fat oxidation and increase thermogenesis. When combined with the caloric-restricting effects of GLP-1, the result is a potent ‘de-fatting’ effect on the liver. The rapid MASH resolution seen here—reaching over 50% in just six months—is highly competitive with other emerging therapies, including resmetirom and tirzepatide.
The failure to meet the fibrosis endpoint at 24 weeks should be interpreted with caution. Fibrosis is a structural change that typically resolves more slowly than inflammation or steatosis. Many clinicians believe that MASH resolution is the necessary precursor to fibrosis regression. The ongoing 48-week portion of this trial will be pivotal in determining if the high rates of MASH resolution eventually translate into significant fibrosis reversal.
Furthermore, the lack of dose titration is a significant clinical advantage. It simplifies the treatment regimen for both patients and providers and allows for the rapid attainment of therapeutic drug levels. However, longer-term data are needed to ensure that the glucagon component does not adversely affect glycemic control in patients with pre-existing type 2 diabetes, although current data suggest the GLP-1 component effectively counterbalances this risk.
Conclusion: The Path Forward for Dual Agonism
The 24-week results of the IMPACT trial position pemvidutide as a promising candidate for the treatment of MASH. By successfully meeting the primary endpoint of MASH resolution with a favorable safety profile and a simplified dosing regimen, it addresses several unmet needs in the field. While the wait for significant fibrosis improvement continues, the rapid reduction in inflammation and steatosis is a strong indicator of therapeutic potential. Future research will focus on the 48-week histological outcomes and the long-term impact on cardiovascular health, which remains the leading cause of mortality in patients with MASH.
Funding and ClinicalTrials.gov
This study was funded by Altimmune. The trial is registered with ClinicalTrials.gov, identifier NCT05989711.
References
Noureddin M, Harrison SA, Loomba R, et al. Safety and efficacy of weekly pemvidutide versus placebo for metabolic dysfunction-associated steatohepatitis (IMPACT): 24-week results from a multicentre, randomised, double-blind, phase 2b study. Lancet. 2025 Dec 6;406(10520):2644-2655. doi: 10.1016/S0140-6736(25)02114-2. Epub 2025 Nov 11. PMID: 41237796.