Key Highlights
- No significant differences were observed in Recurrence-Free Survival (RFS) or Disease-Specific Survival (DSS) between patients undergoing lobectomy, total thyroidectomy, or total thyroidectomy followed by radioactive iodine (RAI) for cN1b papillary thyroid carcinoma.
- The study suggests that the routine application of total thyroidectomy and adjuvant RAI in all patients with lateral neck metastasis may be unnecessary, particularly for those with lower-risk features.
- Independent risk factors for shorter RFS included older age, larger primary tumor size, larger metastatic lymph node size, and the presence of extranodal extension (ENE).
- Personalized surgical strategies may reduce treatment-related morbidity, such as permanent hypoparathyroidism and salivary gland dysfunction, without compromising oncologic safety.
Background: The Shift Toward Personalized Thyroid Cancer Care
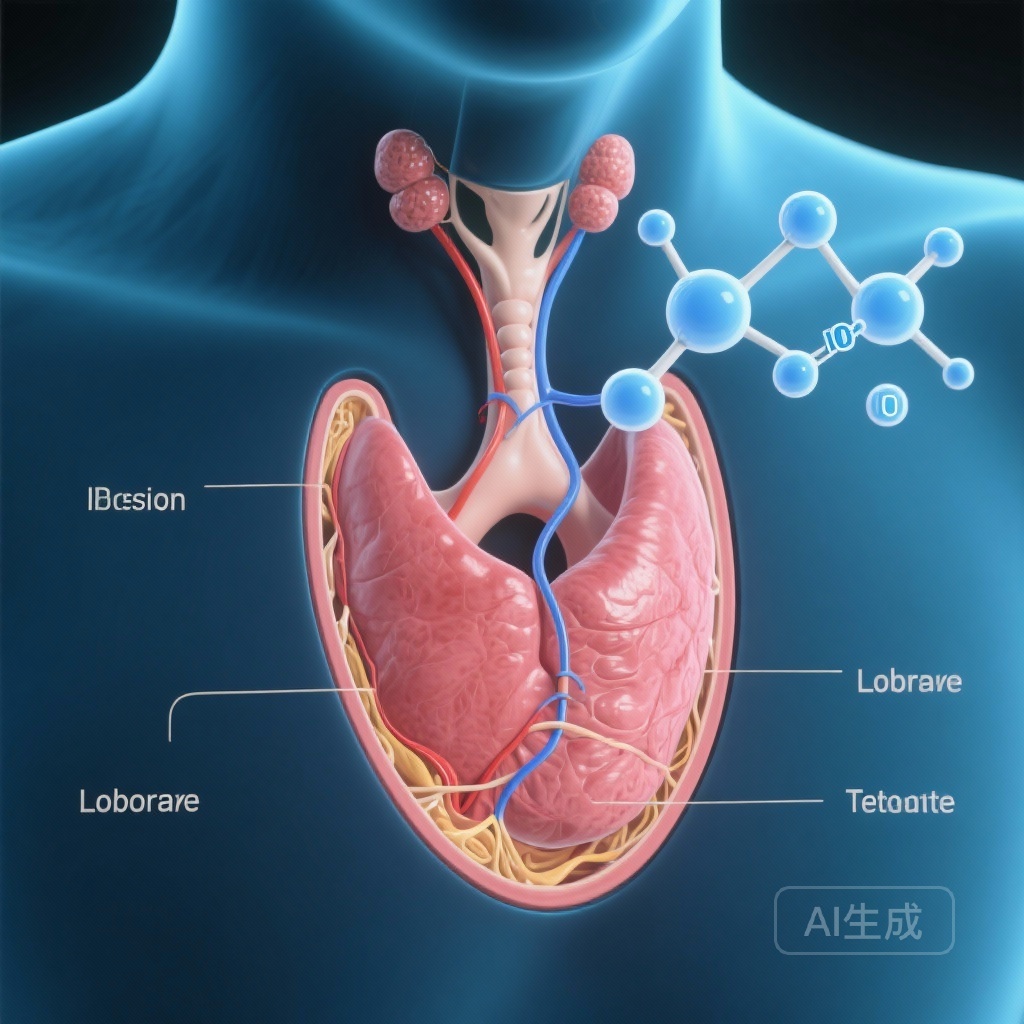
The management of papillary thyroid carcinoma (PTC) has undergone a significant paradigm shift over the last decade. Historically, an aggressive surgical approach followed by radioactive iodine (RAI) ablation was the standard of care for almost all patients. However, as our understanding of tumor biology has evolved, clinical practice has moved toward de-escalation for low-risk disease. The 2015 American Thyroid Association (ATA) guidelines marked a turning point by supporting thyroid lobectomy for T1 and T2 tumors without evidence of extrathyroidal extension or nodal involvement.
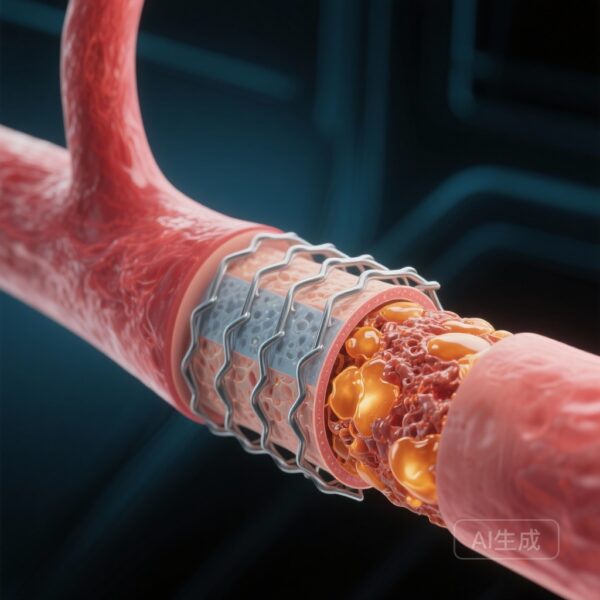
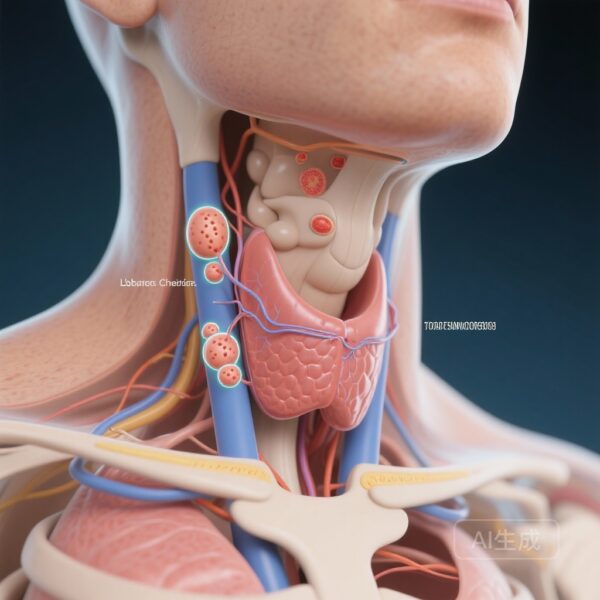
Despite this trend toward conservation, patients presenting with lateral neck metastasis (cN1b) have remained a subgroup for whom aggressive intervention is almost universally recommended. Lateral lymph node involvement is classified as intermediate risk under the ATA risk stratification system, often prompting clinicians to perform a total thyroidectomy (TT) to facilitate subsequent RAI therapy. This approach, while intended to minimize recurrence, carries significant risks, including permanent hypocalcemia, recurrent laryngeal nerve injury, and RAI-induced side effects like sialadenitis. The clinical question remains: Can we safely de-escalate treatment in N1b patients without sacrificing long-term survival?
Study Design and Methodology
In a comprehensive multicenter retrospective cohort study, researchers led by Fujiwara et al. (2025) evaluated the oncologic outcomes of varying treatment intensities in patients with intermediate-risk cN1b PTC. The study included 593 patients treated across multiple institutions between 2010 and 2022. All participants presented with cT1-3N1bM0 disease and underwent therapeutic lateral neck dissection.
The cohort was divided into three primary treatment groups:
- Lobectomy with lateral neck dissection.
- Total thyroidectomy (TT) with lateral neck dissection.
- Total thyroidectomy (TT) with lateral neck dissection followed by adjuvant RAI.
The primary endpoints were Recurrence-Free Survival (RFS) and Disease-Specific Survival (DSS). The researchers utilized Kaplan-Meier analysis to compare survival curves and multivariable Cox proportional hazards models to isolate independent risk factors for recurrence. The median follow-up duration was 71.5 months, providing a robust window for observing oncologic events.
Key Findings: Comparable Outcomes Across Treatment Modalities
The results of the study challenge the conventional wisdom that more aggressive treatment necessarily leads to better outcomes in the N1b population. The analysis revealed no statistically significant differences in RFS (p = 0.19) or DSS (p = 0.40) among the three treatment groups. This finding suggests that for many patients with lateral neck metastasis, the extent of the thyroidectomy and the addition of RAI may not influence the likelihood of recurrence or death.
Interestingly, the group receiving total thyroidectomy plus RAI showed a trend toward worse RFS, although this did not reach statistical significance. This trend likely reflects selection bias, where clinicians were more inclined to prescribe RAI to patients with more aggressive clinical features or higher nodal burdens. However, even when adjusting for these factors, the intensive treatment did not provide a clear survival advantage over more conservative surgical options.
Identifying Independent Risk Factors
Through multivariable analysis, the study identified specific clinical and pathological features that were independently associated with a higher risk of recurrence. These findings are critical for clinicians seeking to identify which N1b patients might still benefit from more intensive monitoring or therapy:
- Older Age: Each year of age was associated with a hazard ratio (HR) of 1.024 for recurrence (p = 0.006).
- Primary Tumor Size: Larger tumor diameter increased the risk of recurrence (HR 1.026 per mm, p < 0.001).
- Metastatic Lymph Node Size: The size of the largest metastatic node was a significant predictor (HR 1.020 per mm, p = 0.017).
- Extranodal Extension (ENE): The presence of ENE was a potent risk factor, nearly doubling the risk of recurrence (HR 1.741, p = 0.033).
Expert Commentary and Clinical Implications
The Fujiwara study adds to a growing body of evidence suggesting that the biology of the tumor and the characteristics of the nodal disease are more important than the radicality of the surgery itself. In patients with cN1b disease who lack high-risk features—such as extranodal extension or a high volume of large metastatic nodes—lobectomy appears to be an oncologically safe alternative to total thyroidectomy.
The clinical implications of these findings are substantial. By opting for lobectomy in selected N1b cases, surgeons can significantly reduce the risk of permanent hypoparathyroidism, which remains one of the most debilitating complications of thyroid surgery. Furthermore, avoiding unnecessary RAI prevents long-term morbidity, including salivary gland damage and the small but non-negligible risk of secondary malignancies.
However, it is essential to interpret these findings with caution. This was a retrospective study, and the selection of treatment was at the discretion of the treating physicians, which introduces inherent bias. The study also highlights that RAI may still have a role in patients with extensive nodal disease or high-risk pathological features like ENE. The goal of modern thyroid oncology is not to avoid treatment, but to ensure that the intensity of the treatment matches the risk profile of the individual patient.
Conclusion: A Path Toward Selective Treatment
The findings from this multicenter study support a more nuanced, risk-stratified approach to N1b papillary thyroid carcinoma. While total thyroidectomy and RAI have long been the default for lateral neck metastasis, this data suggests that lobectomy with lateral neck dissection can achieve equivalent oncologic outcomes in many intermediate-risk patients. Future prospective trials and longer-term follow-up will be necessary to further refine the criteria for de-escalation, but for now, clinicians have a strong evidentiary basis to discuss more conservative, personalized surgical options with their patients.
References
Fujiwara T, Kofuji N, Kishimoto Y, Hamaguchi K, Shinohara S, Kikuchi M, Asato R, Ishida H, Kitani Y, Otsuki S, Kusano J, Tsujimura T, Harada H, Yasuda K, Tamaki H, Omori K. Are Total Thyroidectomy and Adjuvant Radioactive Iodine Treatment Required in All Patients with N1b Intermediate-High Risk Papillary Thyroid Carcinoma? Thyroid. 2025 Dec 4. doi: 10.1177/10507256251401241. Epub ahead of print. PMID: 41371750.